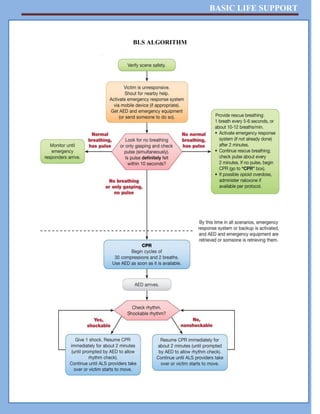
This document is an informational booklet on Basic Life Support (BLS), detailing essential skills for saving lives during cardiac arrest, including CPR techniques and the chain of survival. It covers heart anatomy, cardiac arrest causes, symptoms, diagnosis, and management, as well as steps for performing CPR and using automated external defibrillators (AED). The content emphasizes the importance of quick recognition and response to cardiac emergencies to enhance survival rates.