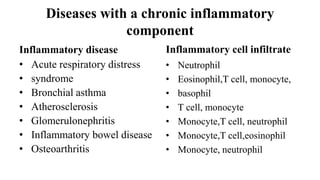
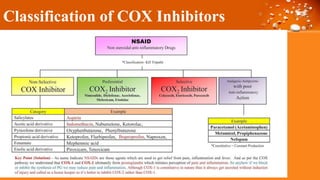
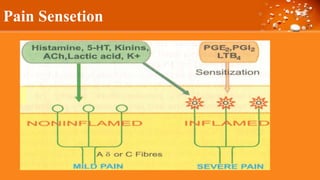
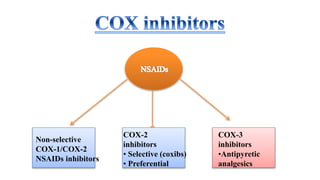
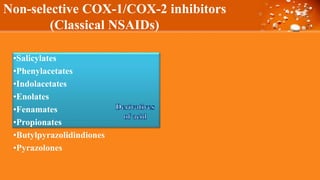
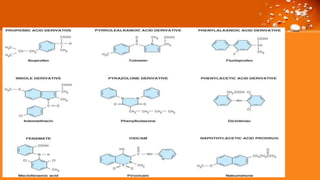
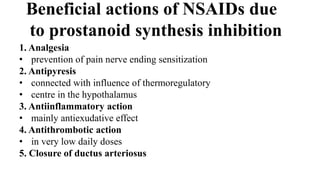
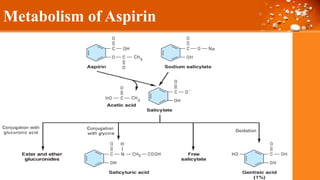
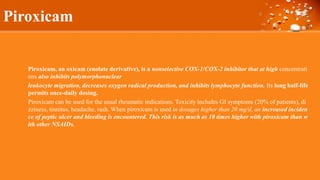
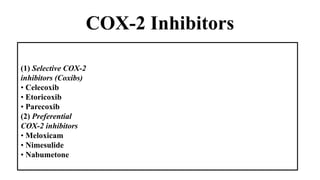
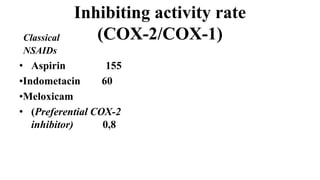
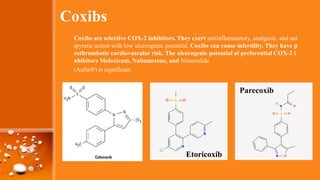
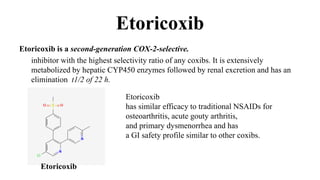
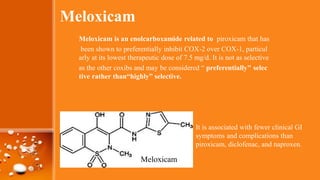
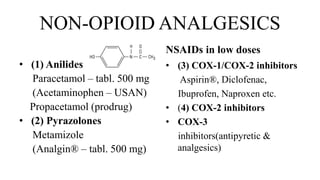
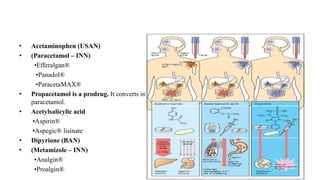
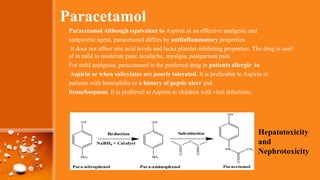
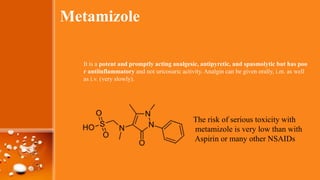
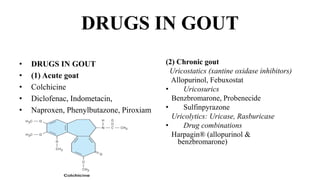
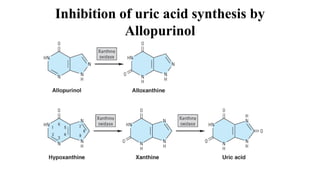
This document discusses cyclooxygenase (COX) inhibitors, focusing on their role in managing chronic pain syndromes and their classification in pharmacology. It covers their mechanisms of action, indications, adverse effects, and contraindications, highlighting the differences between COX-1 and COX-2 inhibitors. Additionally, it provides insights into specific medications within these categories and their applications in pain management and treatment of conditions such as arthritis and gout.