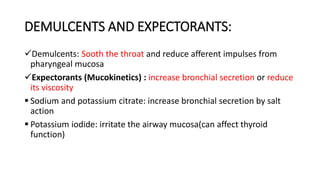
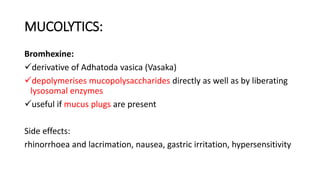
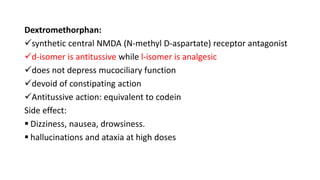
This document discusses different types and classifications of cough medications. It describes demulcents which soothe the throat, expectorants which increase bronchial secretions or reduce viscosity, and mucolytics which break down mucus. It also discusses antitussives which suppress the cough center or act peripherally, including opioids, nonopioids, antihistamines, and prenoxdiazine. Bronchodilators are described as adjuvant antitussives by improving airflow during coughing.