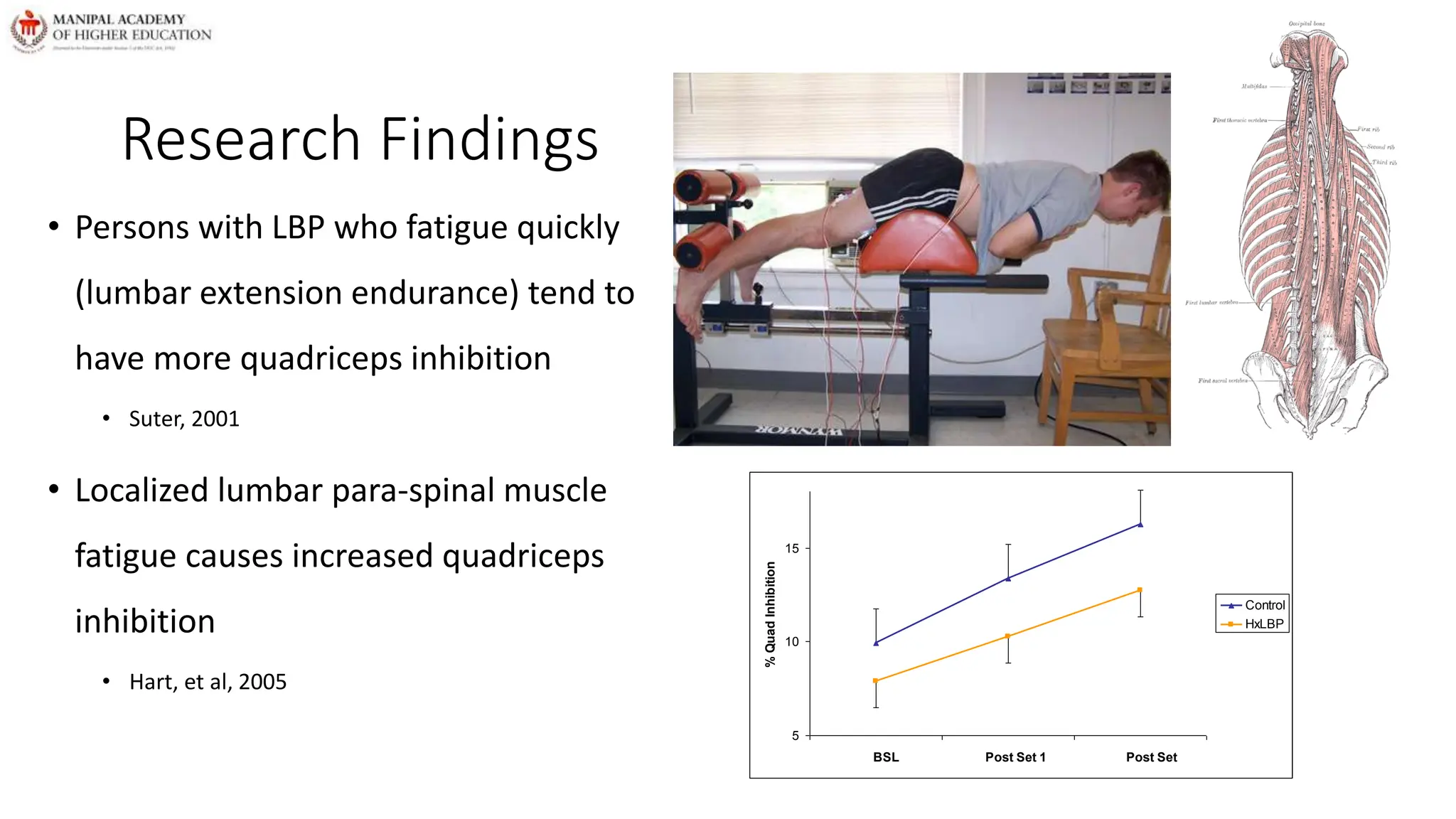
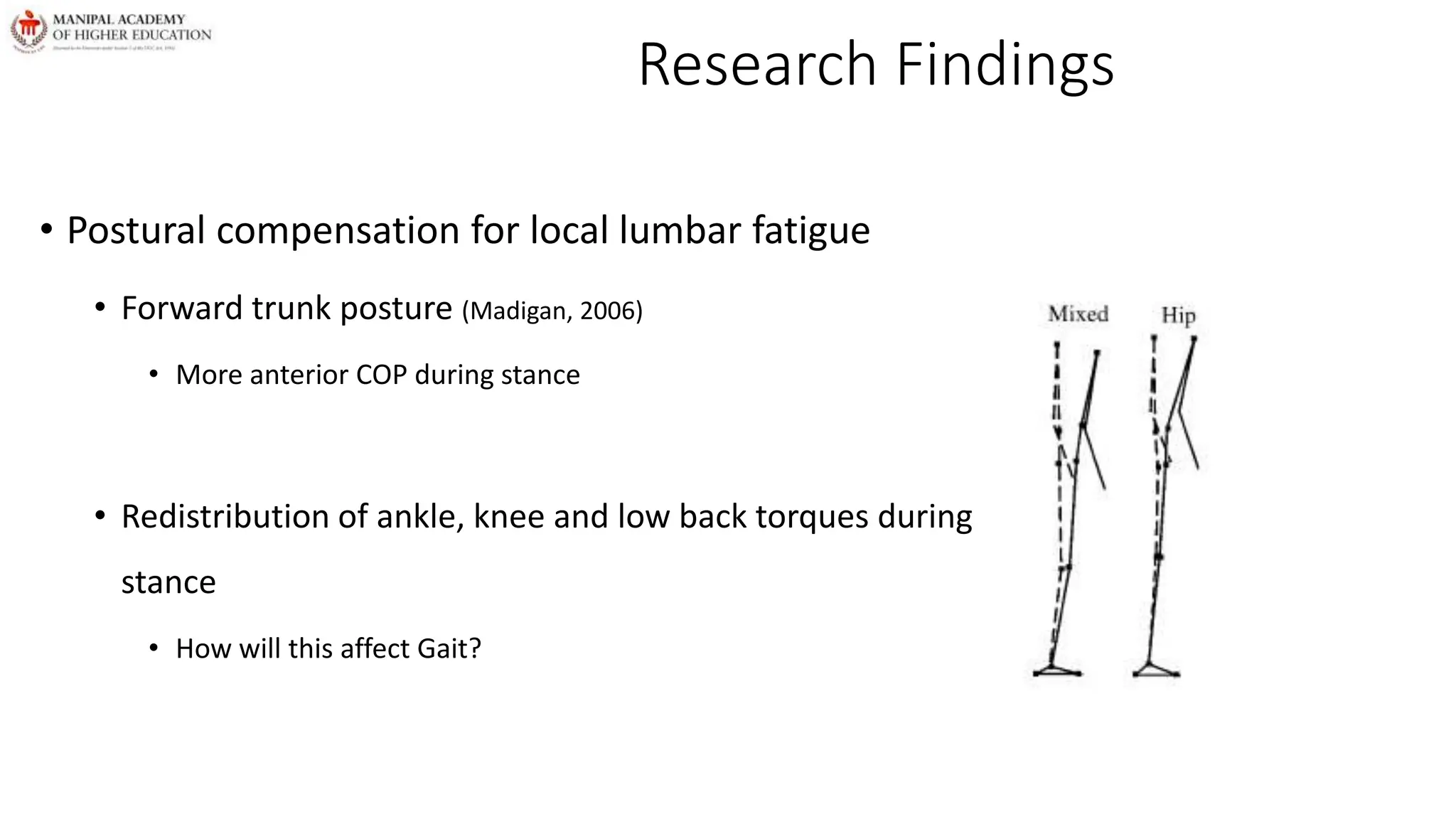
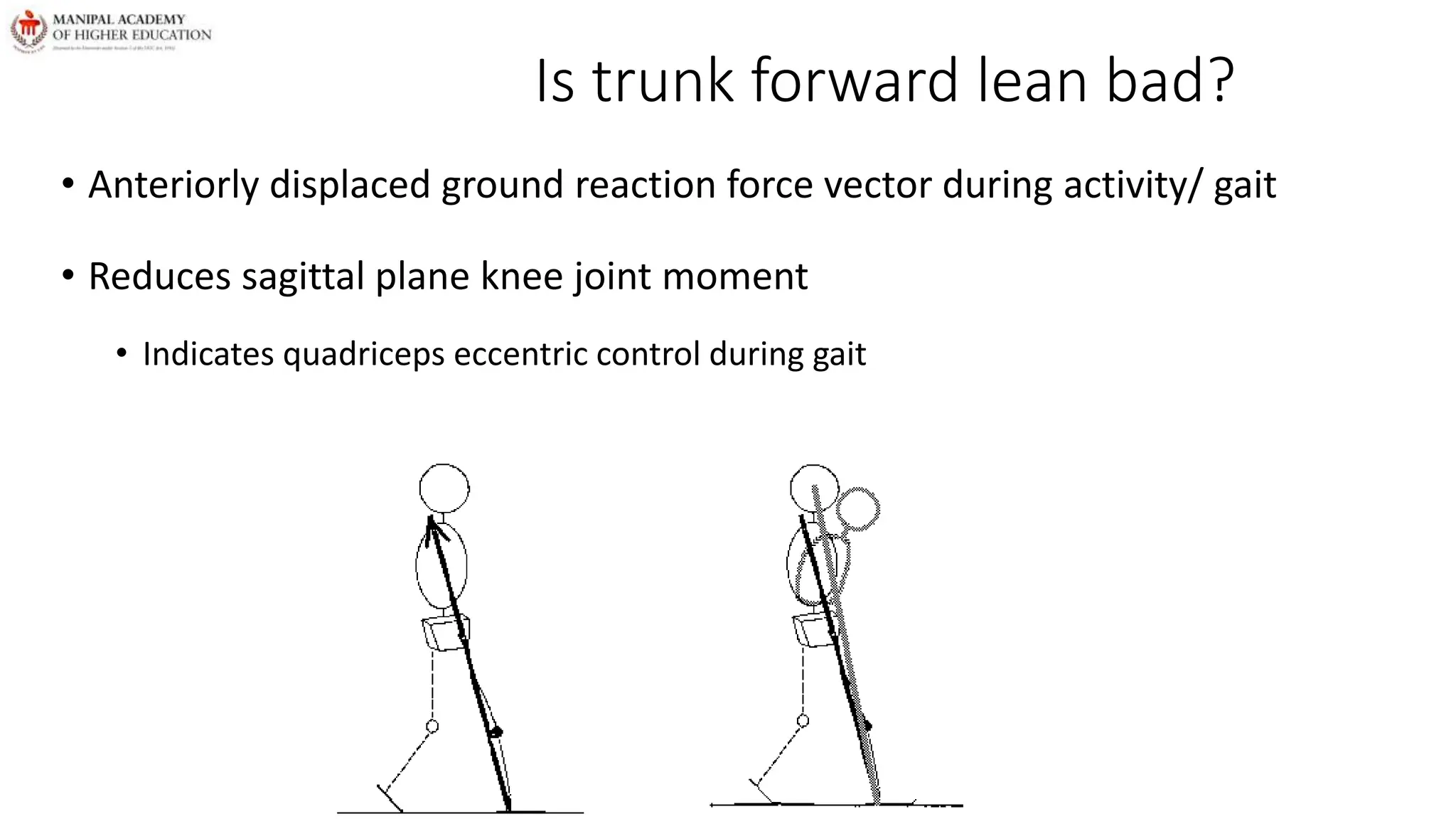
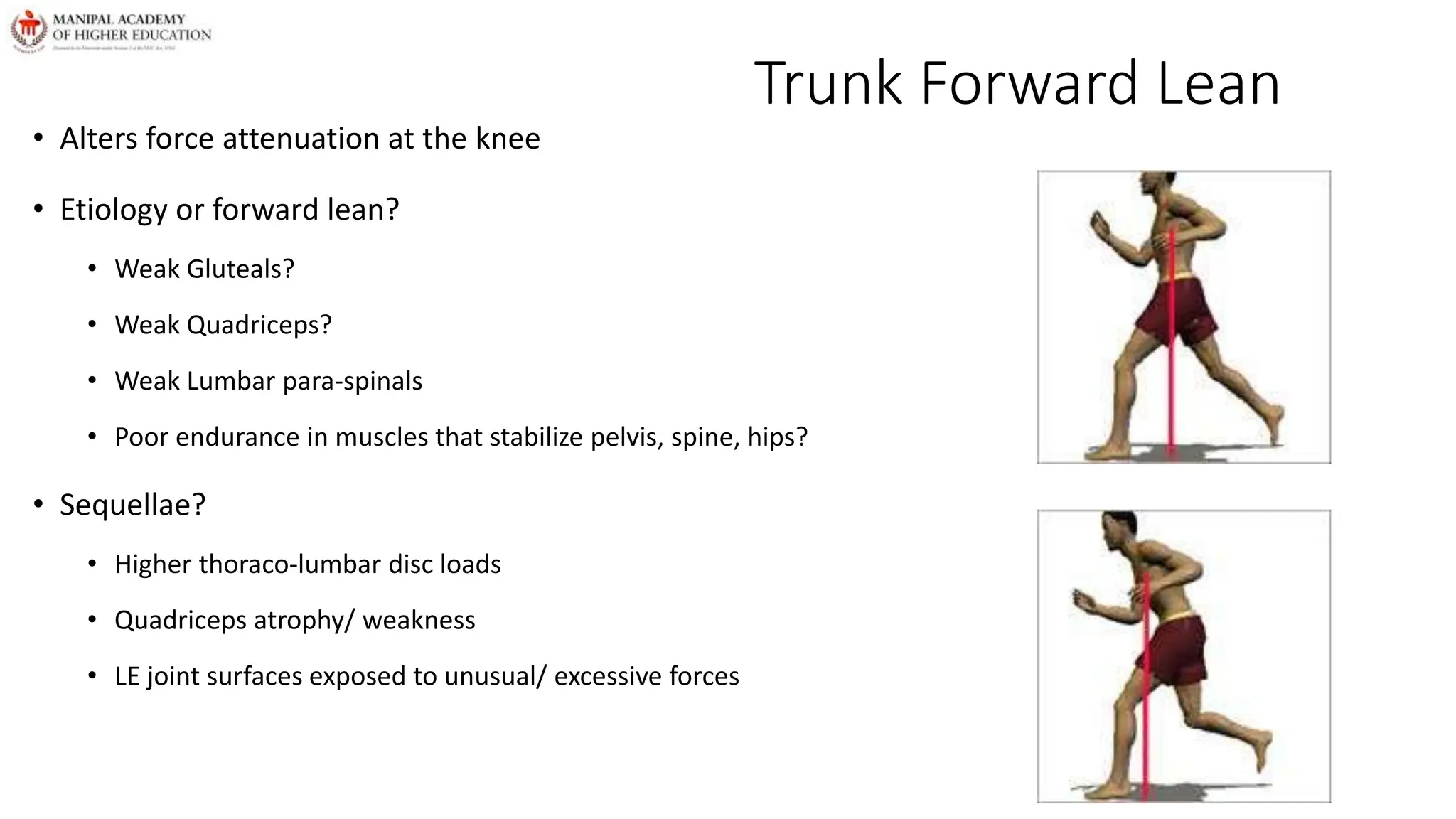
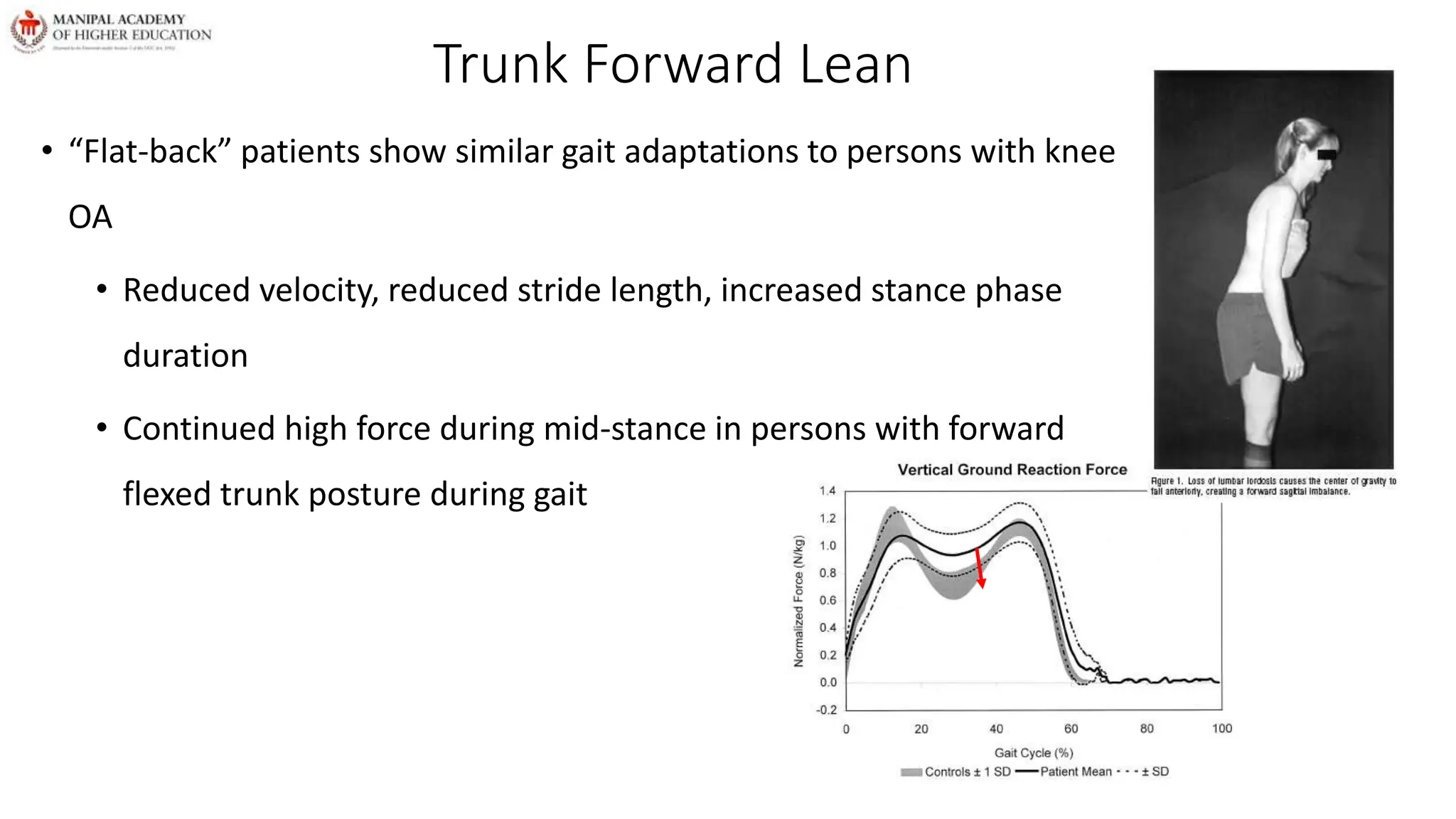
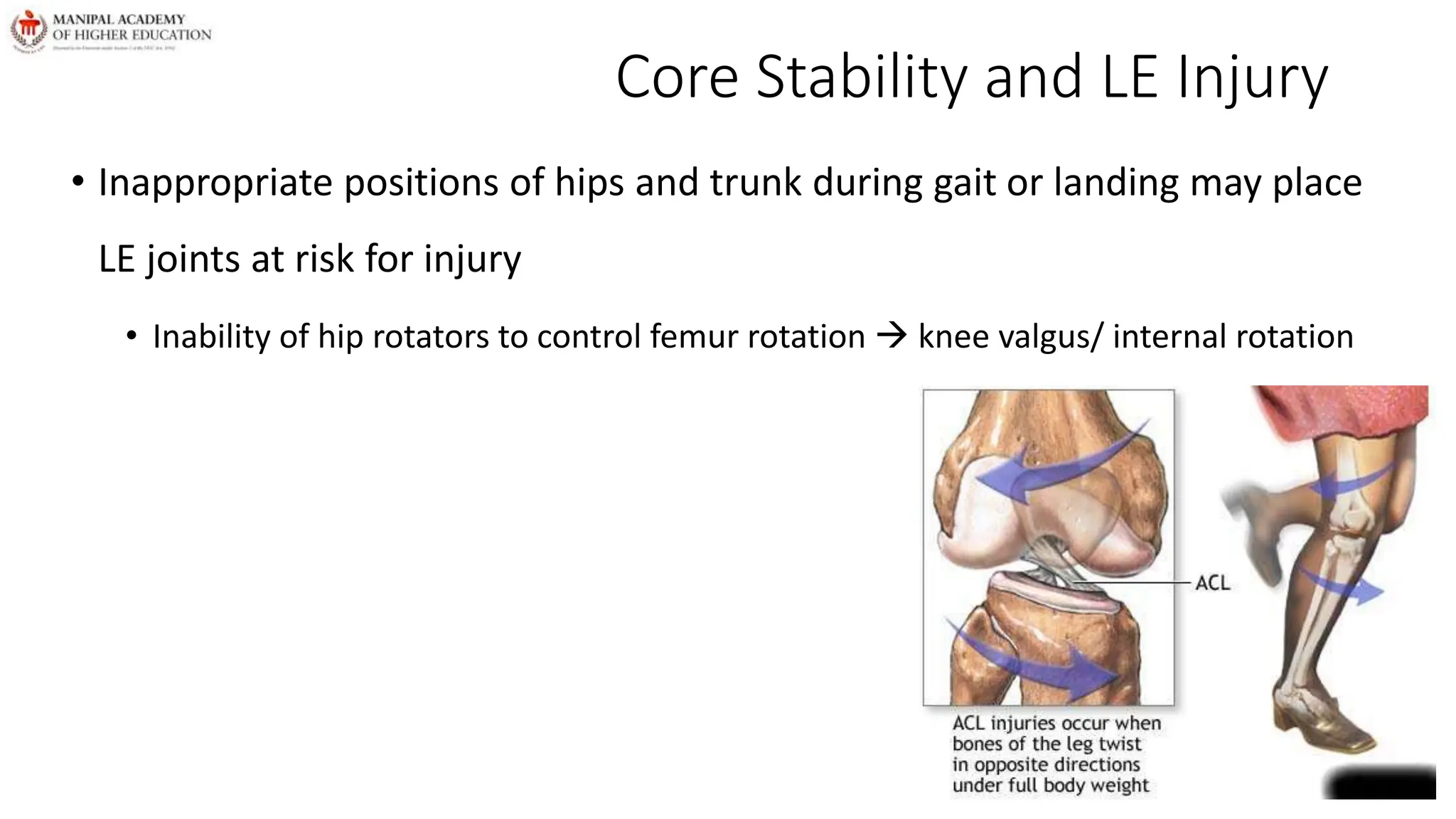
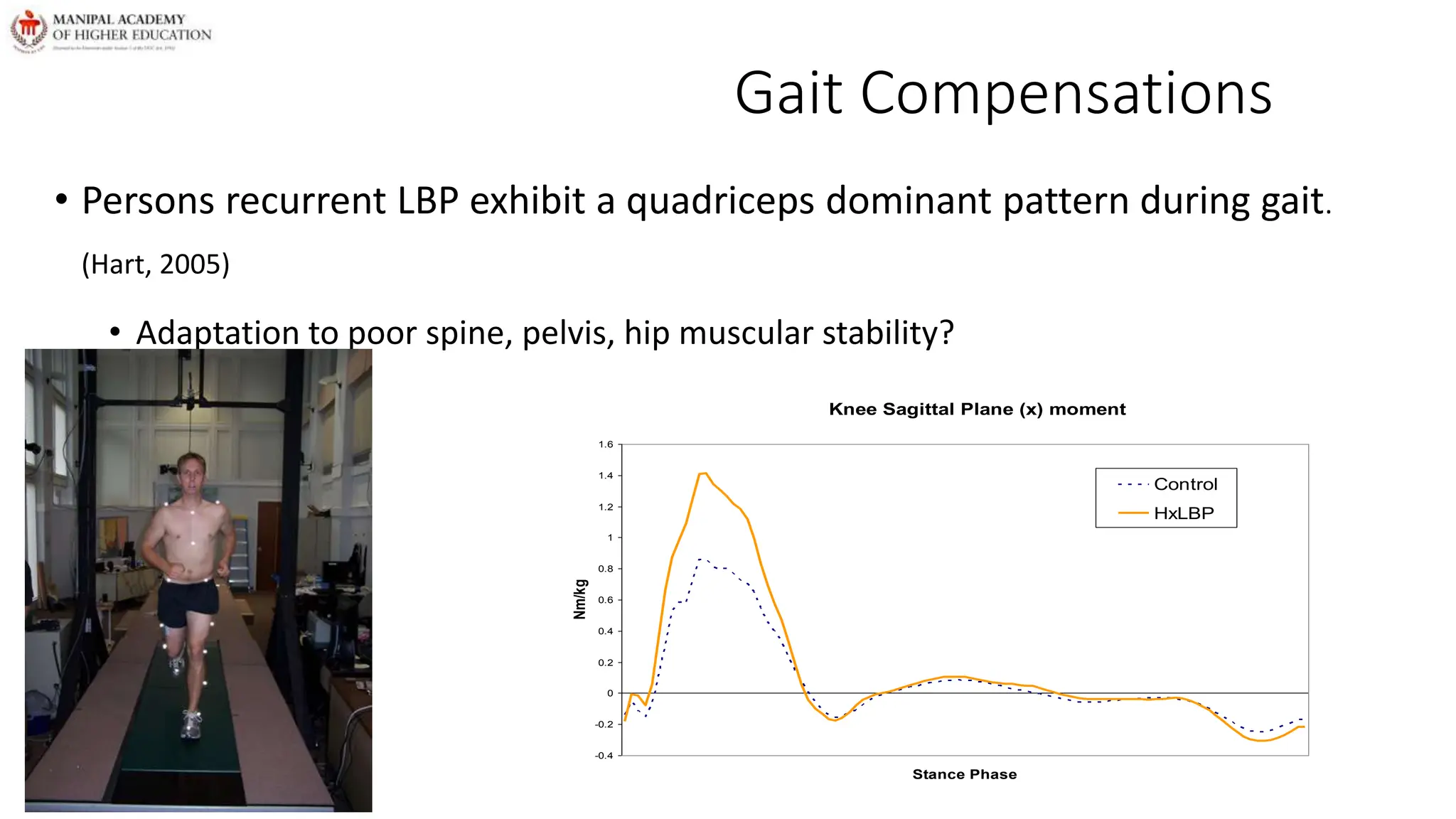
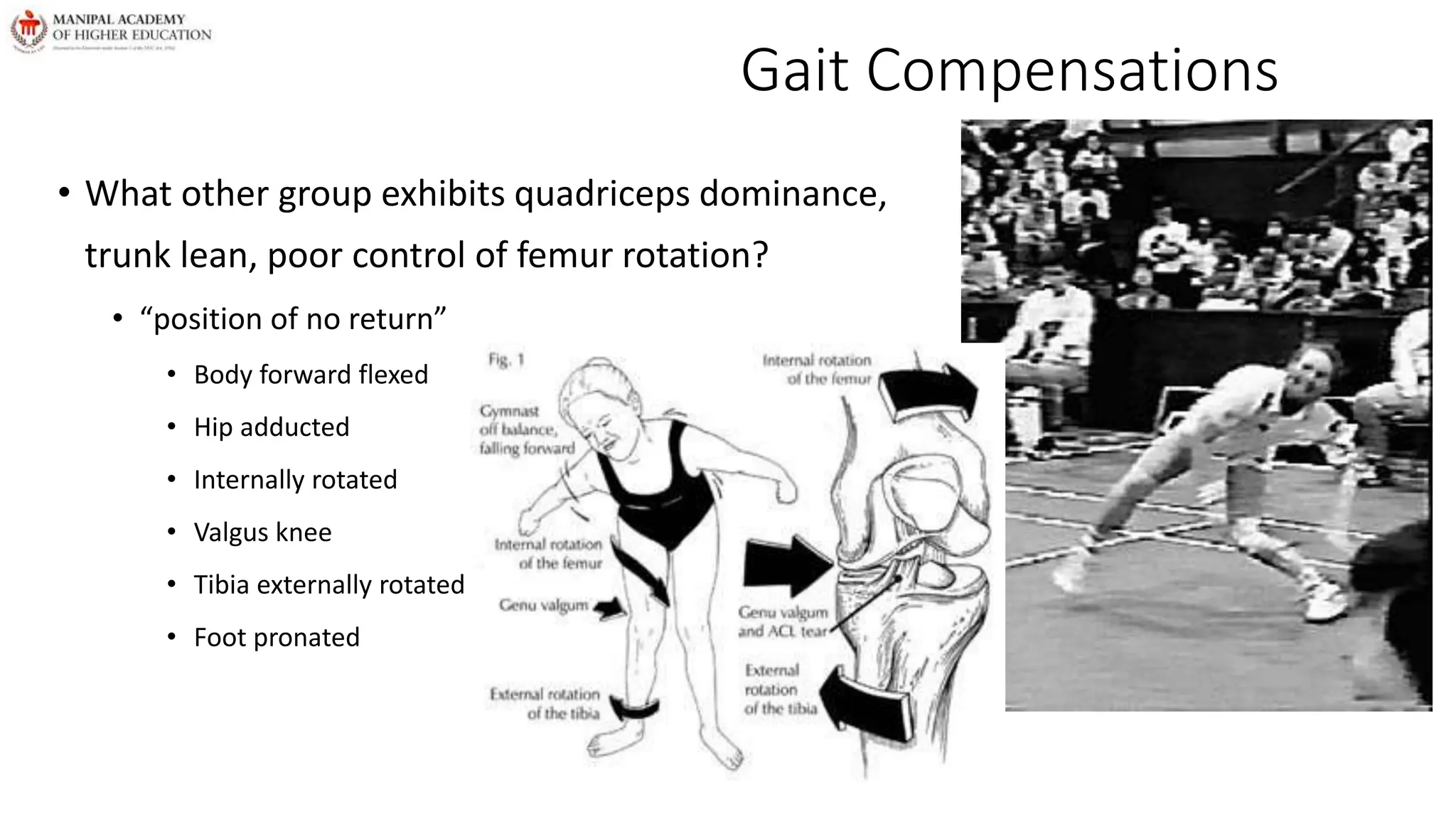
Core dysfunction can lead to lower extremity consequences due to poor stability of the lumbo-pelvic-hip complex. Fatigue of core muscles results in altered trunk and lower extremity biomechanics during gait like forward trunk lean, increased knee and hip flexion, and over-reliance on the quadriceps. This places increased stress on the knees and can increase injury risk. Core stability exercises in children help develop a stable base for motor development and allow them to focus on tasks.






![Muscle activation in child’s legs with and without spasticity following backward translation of the platform
(vertical arrow).
Note the reversal in muscle onset sequencing (horizontal arrows) in the leg with spasticity [HAMSTRINGS
BEING ACTIVATED PRIOR TO GASTROCNEMIUS] (Nashner, Shumway-Cook, & Marin, 1983)](https://image.slidesharecdn.com/coredsfunctin-240404082344-2af99854/75/Core-Dysfunction-in-children-with-CP-pptx-37-2048.jpg)
![Recommended Interventions
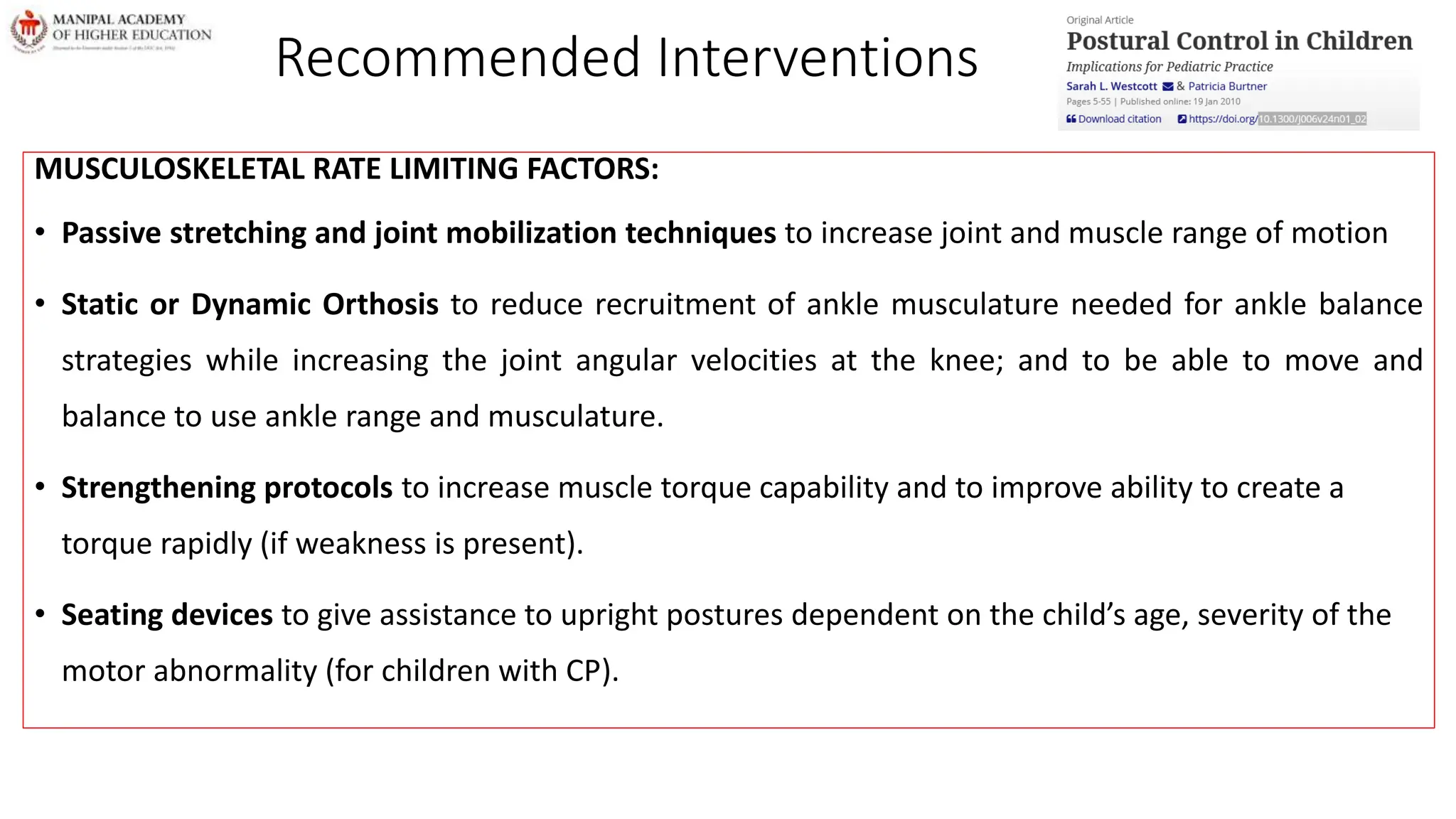
MOTOR PROCESSES RATE LIMITING FACTORS:
• Modify environment and task to practice the strategy not used (e.g., provoking use of an ankle strategy when a hip
strategy is primarily used by the child via roller skating) or to provoke a more optimal strategy.
• Practice in reaching to the limits of stability and reaching quickly for children who actively use co-contractions and limit
their movement speed and the distance of COG displacement, so as to not challenge stability. Reaching in reaction to an
external stimulus (ball thrown to child) can be used to provoke faster reach movement and higher amplitude APA.
• Practice reaching with the hand weighted to provide increased proprioception and potential strengthening, and
additionally increased duration of APA in this practice (Bouisset, Richardson, & Zattara, 2000).
• Practice of posture and movement with feedback about posture (using mirrors, auditory input [bells, squeak toys], lights,
or electrical stimulation to cue the child to change starting positions) will affect the RPA and APA for motor coordination
pattern of the movement task.](https://image.slidesharecdn.com/coredsfunctin-240404082344-2af99854/75/Core-Dysfunction-in-children-with-CP-pptx-39-2048.jpg)