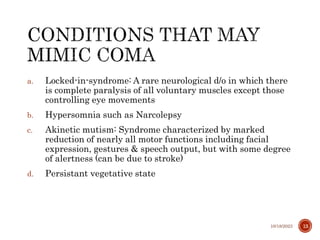
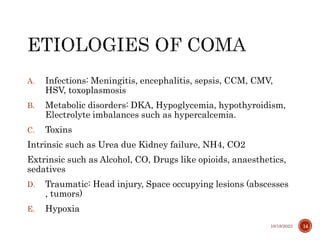
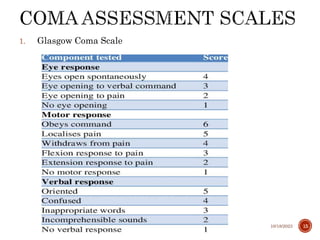
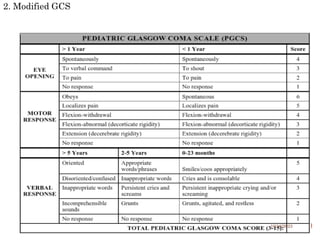
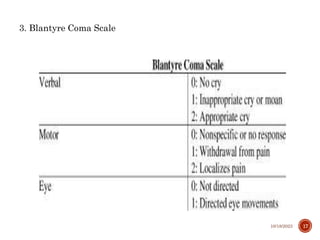
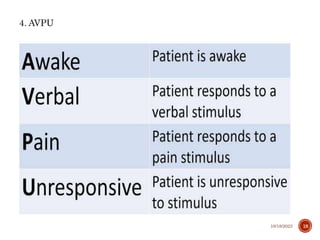
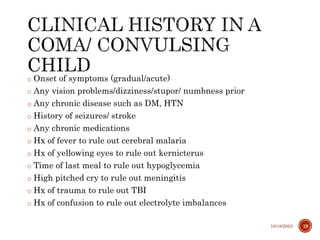
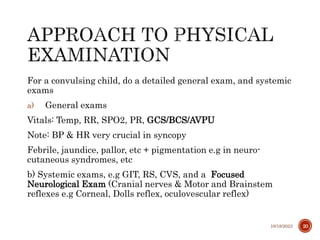
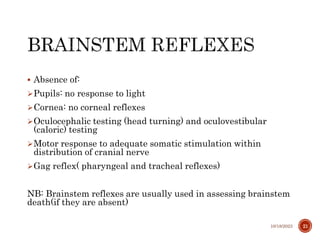
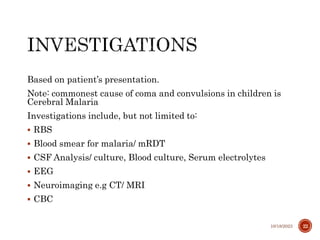
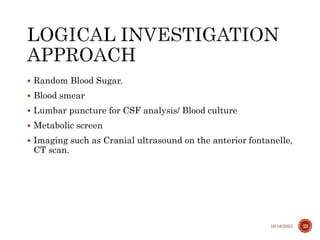
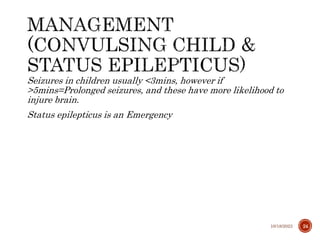
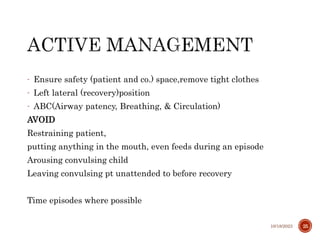
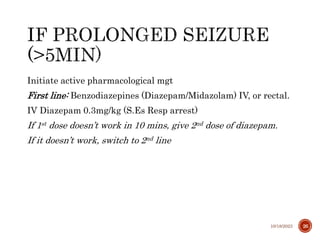
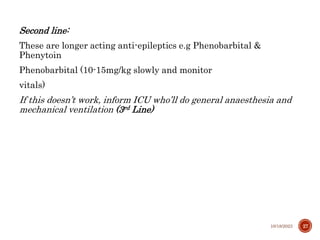
This document provides definitions and discusses the neuroanatomy, physiology, etiologies, assessment scales, approach, investigations, and management of coma and seizures in children. It begins with definitions of key terms like seizure, fit, spasm, convulsions, coma, epilepsy, and status epilepticus. It then covers the neuroanatomy of normal consciousness versus coma, conditions that mimic coma, and common etiologies of coma. Assessment scales for coma like the Glasgow Coma Scale and Blantyre Coma Scale are also defined. The document outlines the approach to a convulsing or comatose child, including history and physical exam considerations, as well as common investigations. It concludes