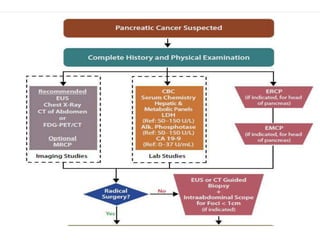
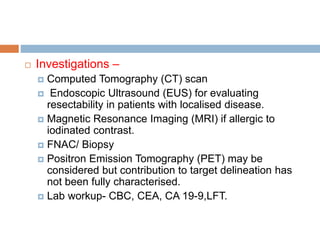
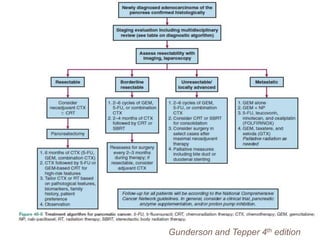
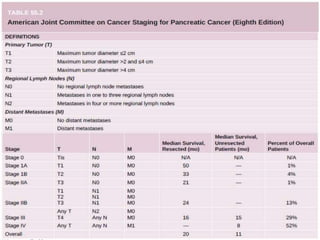
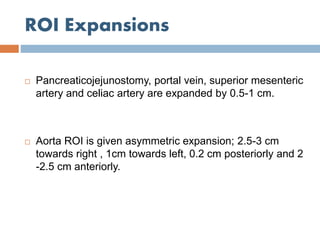
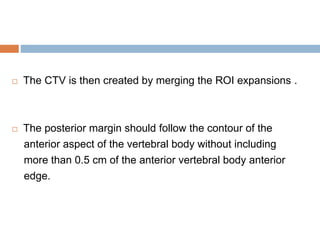
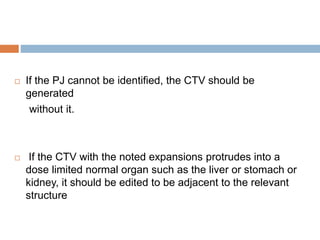
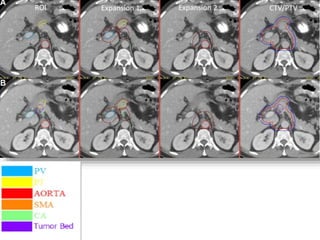
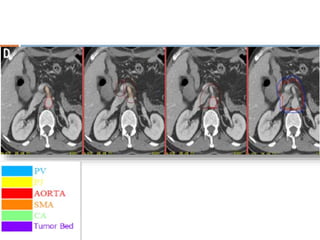
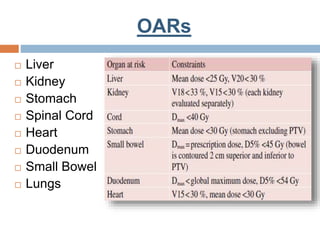
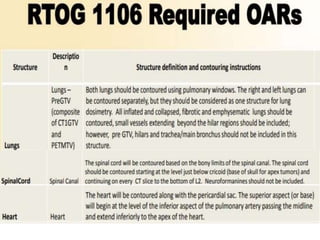
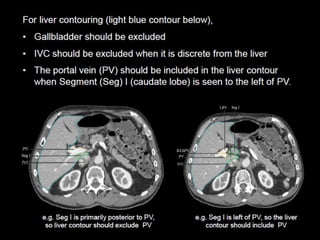
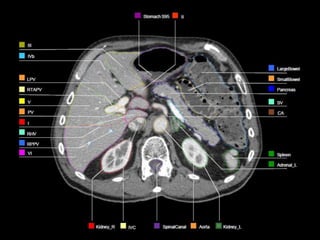
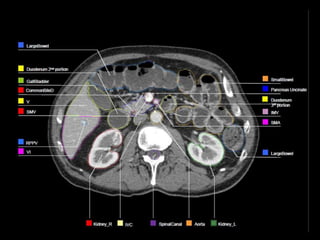
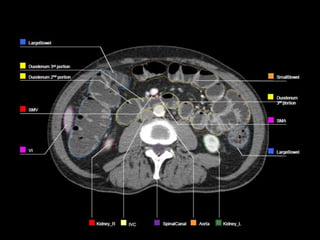
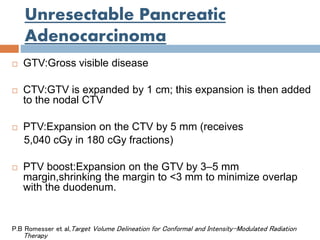
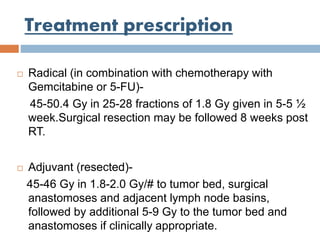
This document provides contouring guidelines for pancreatic malignancies. It discusses the anatomy, risk factors, clinical presentation, investigations, and target volume delineation for resected pancreatic cancer and unresectable pancreatic adenocarcinoma. Target volumes include the postoperative tumor bed, anastomoses, abdominal nodal regions, and organs at risk. The treatment prescription for radical and adjuvant settings is also outlined.