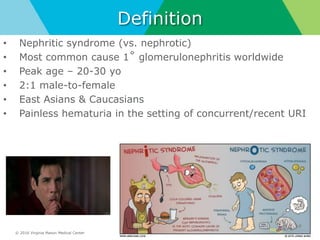
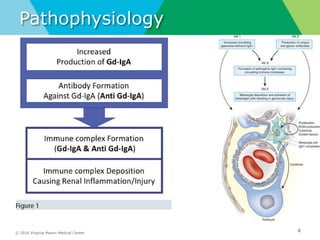
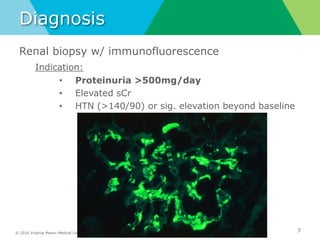
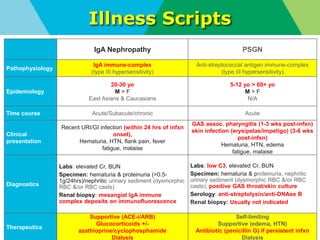
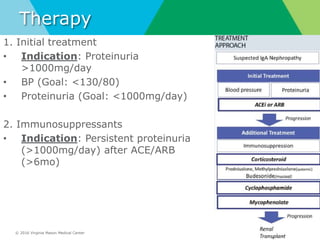
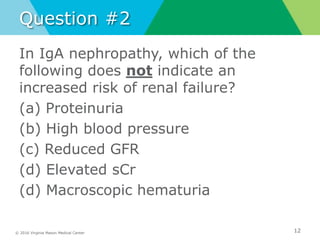
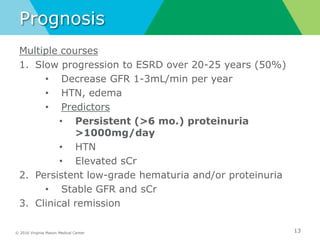
IgA nephropathy (Berger's disease) is the most common cause of primary glomerulonephritis worldwide. It is characterized by IgA immune complex deposition in the mesangial areas of the kidneys. Clinical presentation includes gross or microscopic hematuria, often following an upper respiratory or gastrointestinal infection. Diagnosis is made by renal biopsy showing mesangial IgA deposits on immunofluorescence. Treatment focuses on controlling blood pressure and reducing proteinuria with ACE inhibitors, ARBs, or immunosuppressants. Prognosis depends on the degree of proteinuria and hypertension, with many patients experiencing slow progression to end-stage renal disease over 20-25 years.