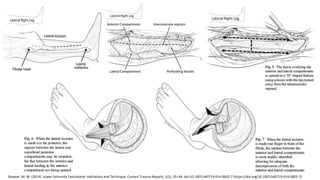
Compartment syndrome is a medical condition caused by increased pressure within a compartment in the body that reduces blood flow. Left untreated, it can lead to muscle and nerve damage or even limb loss. The document discusses compartment syndrome specifically in the lower extremity. It defines compartment syndrome, outlines risk factors, describes the pathophysiology and classic symptoms, and provides guidance on diagnosis using compartment pressure measurements. It also details the preferred surgical treatment of a two incision four compartment fasciotomy and emphasizes proper wound care after to minimize skin retraction and allow tissue recovery.

![Pathophysiology
Inadequate
perfusion
Decreasing the
arteriovenous gradient
Increase in venous &
tissue pressure
Local tissue
edema
Volume increase
Bleeding/
inflammation
Trauma
Further increases to
vessel wall
permeability
Anoxic damage to
endothelial cells
Ischemic changes
Muscle necrosis
Local edema and
pressure increases
Tillinghast CM, Gary JL. Compartment Syndrome of the Lower Extremity. 2019 Sep 3. In:
Mauffrey C, Hak DJ, Martin III MP, editors. Compartment Syndrome: A Guide to Diagnosis
and Management [Internet]. Cham (CH): Springer; 2019. Chapter 8. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK553915/ doi: 10.1007/978-3-030-22331-1_8](https://image.slidesharecdn.com/compartmentsyndrome-220906235530-2c99b68e/85/Compartment-Syndrome-pptx-6-320.jpg)
![Diagnosis
Classic signs of the 5 ‘P’s’:
Pain, mostly pain on passive stretch
Paresthesia
Pallor
Paralysis,
and Pulselessness
Intramuscular compartment pressure: N: < 30 mmHg
Tissue/muscle perfusion pressure (delta pressure):
which is calculated as diastolic blood pressure minus the
compartment pressure
N: > 30 mmHg
Cone J, Inaba K. Trauma Surg Acute Care Open 2017;2:1–6. doi:10.1136/tsaco-2017-000094
Tillinghast CM, Gary JL. Compartment Syndrome of the Lower Extremity. 2019 Sep 3. In: Mauffrey C, Hak DJ, Martin III MP, editors. Compartment Syndrome: A Guide to Diagnosis
and Management [Internet]. Cham (CH): Springer; 2019. Chapter 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553915/ doi: 10.1007/978-3-030-22331-1_8](https://image.slidesharecdn.com/compartmentsyndrome-220906235530-2c99b68e/85/Compartment-Syndrome-pptx-8-320.jpg)

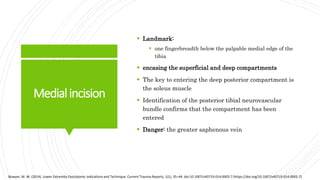
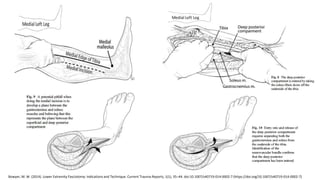
![WoundCare
Focuses on swelling control, allowing recovery of
injured tissues, and minimizing skin retraction.
Dressing changes, re-evaluation of muscle viability,
and gradual closure of the wound every 24 to 72 h
Fasciotomy performed for both therapeutic and
prophylactic purposes should be managed as an open
wound during the first 2–3 days followed by a primary
closure of the wound (Alkhalifah & Almutairi, 2019)
Wound closure options:
Vessel-loop or shoelace technique
Dynamic dermatotraction
Subatmospheric (negative pressure) wound dressings
If the wounds cannot be primarily closed within 7–10
days split-thickness skin grafts (STSG)
Bowyer, M. W. (2014). Lower Extremity Fasciotomy: Indications and Technique. Current Trauma Reports, 1(1), 35–44. doi:10.1007/s40719-014-0002-7
Alkhalifah, M. K., & Almutairi, F. S. H. (2019). Optimising Wound Closure Following a Fasciotomy: A narrative review. Sultan Qaboos University Medical Journal
[SQUMJ], 19(3), e192–200. https://doi.org/10.18295/squmj.2019.19.03.004](https://image.slidesharecdn.com/compartmentsyndrome-220906235530-2c99b68e/85/Compartment-Syndrome-pptx-16-320.jpg)