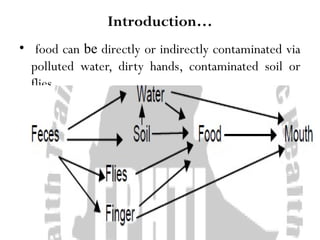
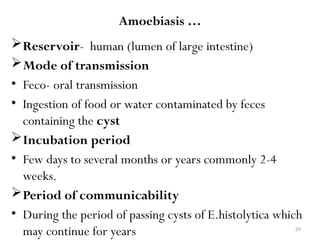
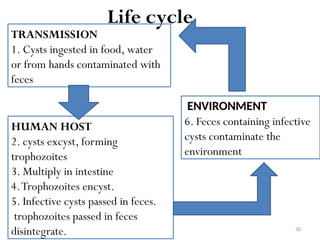
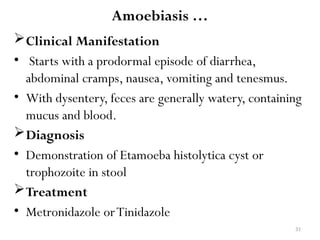
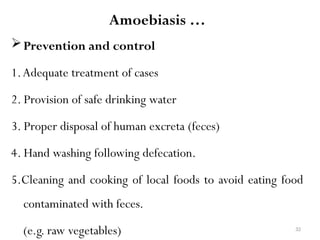
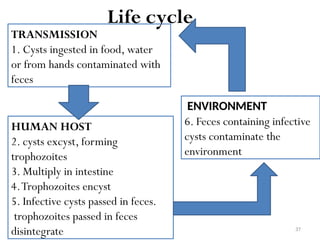
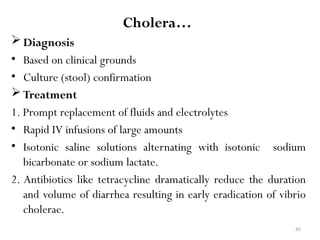
The document discusses oral-fecal transmitted diseases, focusing on their transmission routes, causative organisms, clinical manifestations, diagnosis, treatment, and prevention strategies. Key diseases covered include typhoid fever, bacillary dysentery, amoebiasis, giardiasis, cholera, and infectious hepatitis, emphasizing the importance of hygiene and safe water supply to control outbreaks. The document highlights the role of five key 'Fs' (finger, flies, food, fomites, and fluid) in the transmission and advocates for public health education to prevent these diseases.