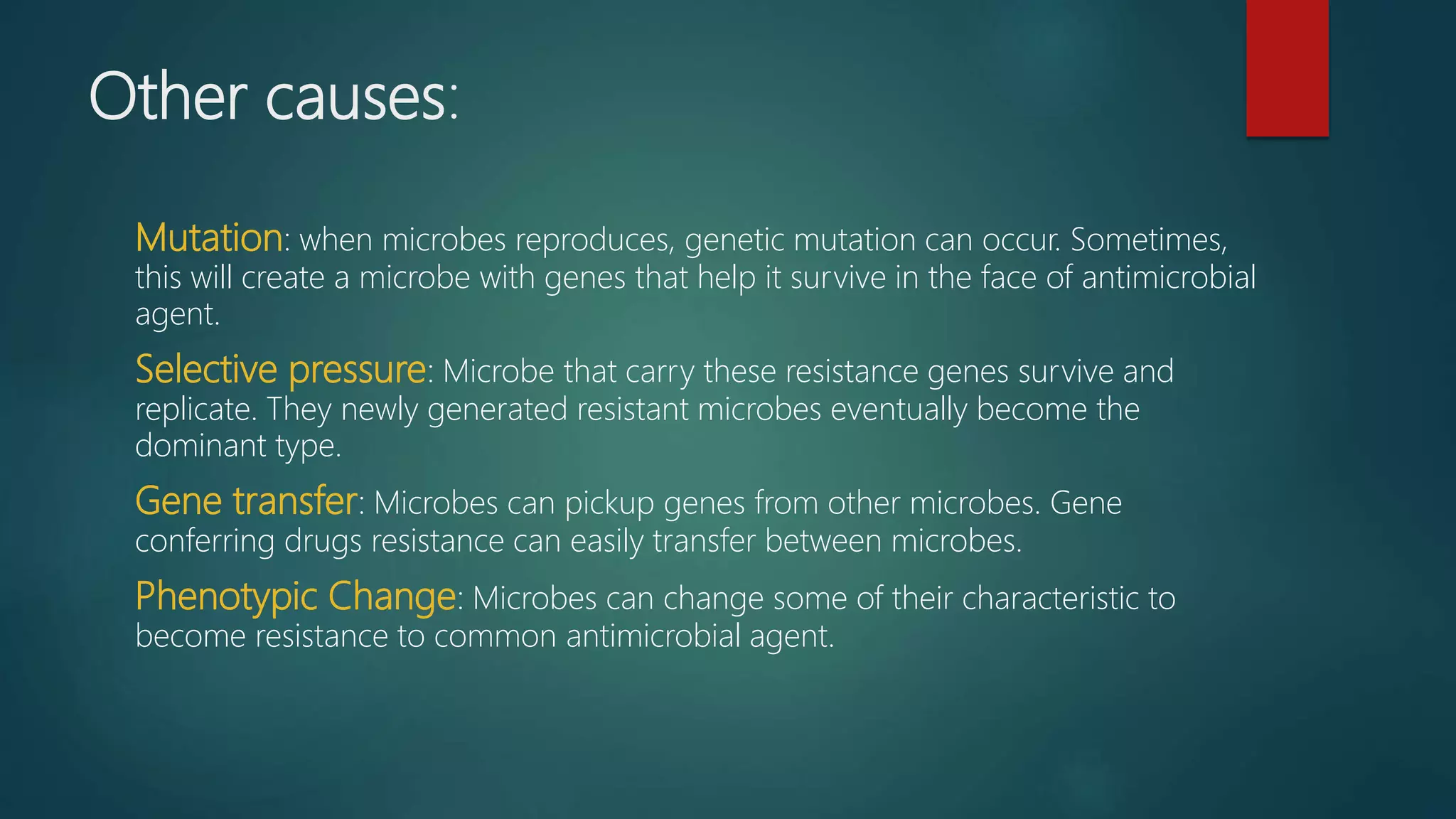
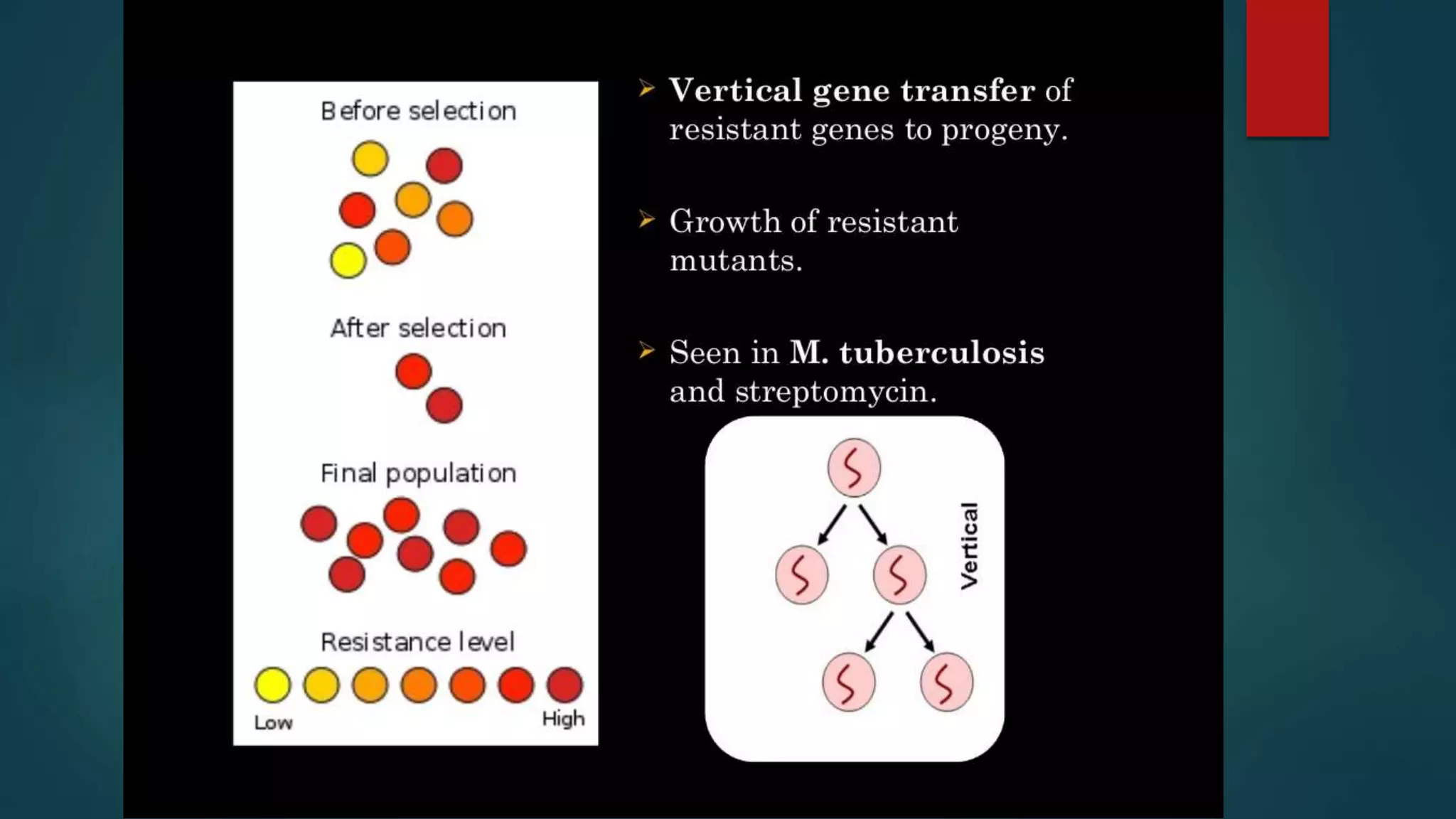
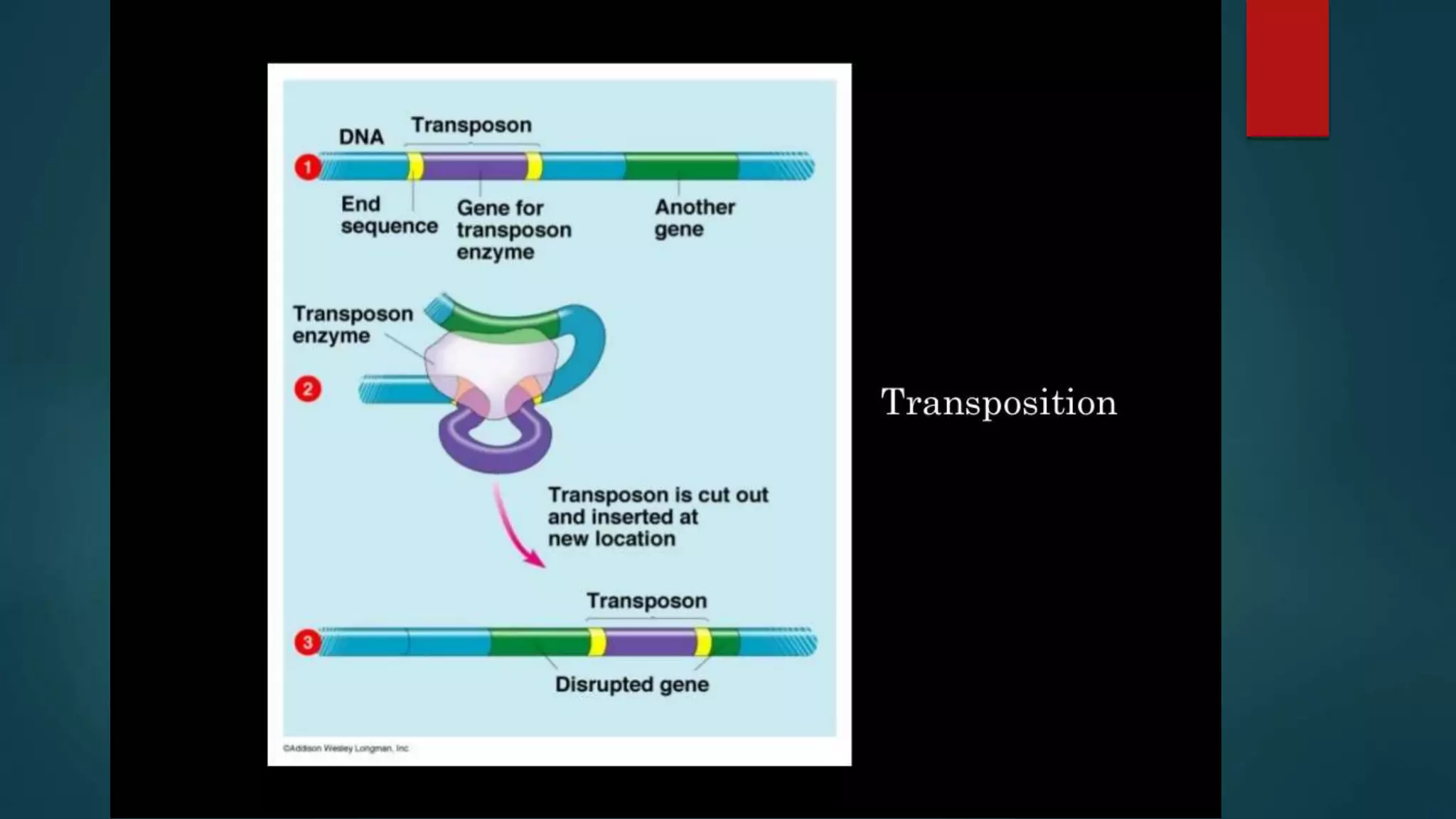
Drug resistance occurs through several mechanisms: mutation, selective pressure, and gene transfer allow microbes to develop resistance. Strategies to combat resistance include international collaboration on surveillance and incentives for new drugs, national treatment guidelines and education programs, and community efforts like rational antibiotic use and hygiene. Genetic changes allow microbes to develop resistance through various mechanisms like mutation, selective pressure, and horizontal gene transfer between microbes.