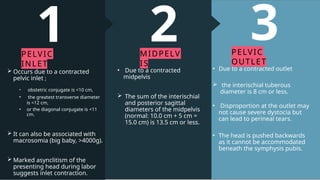
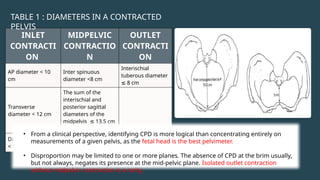
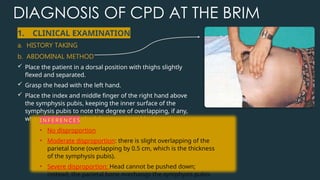
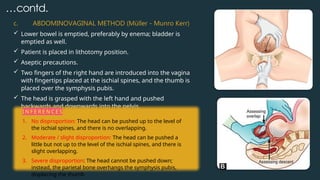
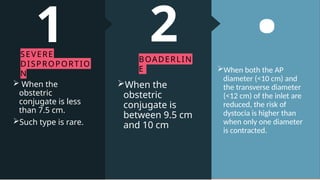
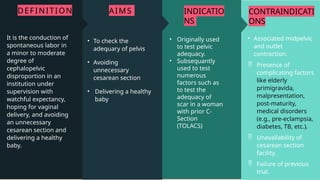
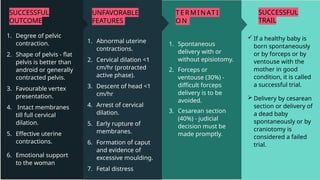
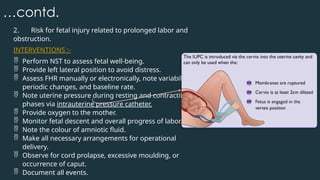
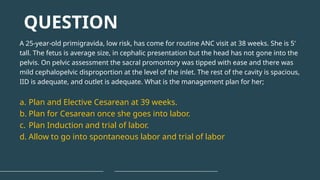
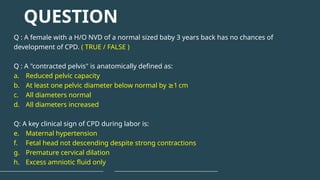
Cephalopelvic Disproportion (CPD) is a condition where the fetal head is too large to pass through the maternal pelvis due to either a large fetal head, a small maternal pelvis, or a combination of both.
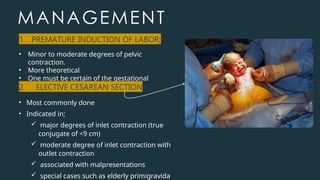
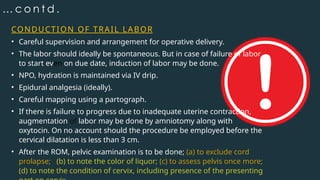
Cephalopelvic Disproportion (CPD) remains one of the important complications during labor. Timely recognition and appropriate identification are essential to ensure maternal and fetal safety. CPD refers to a mismatch between the size of the fetal head and the maternal pelvis, preventing the head from engaging or descending despite strong uterine contractions. This can prolong labor, lead to fetal distress, or require operative delivery.