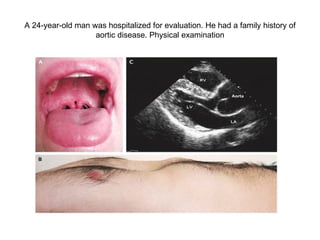
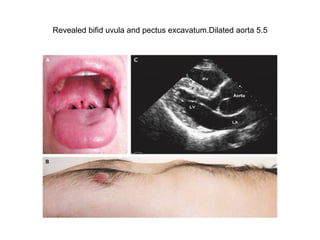
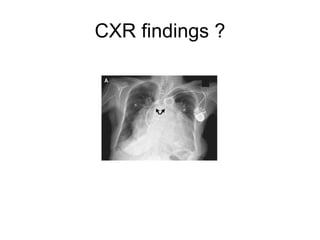
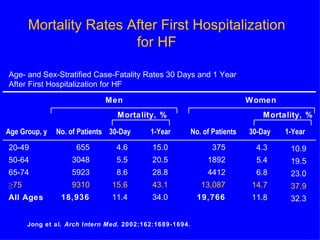
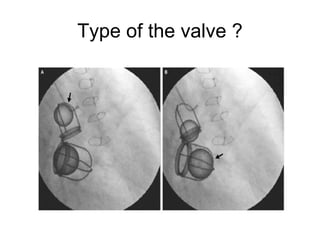
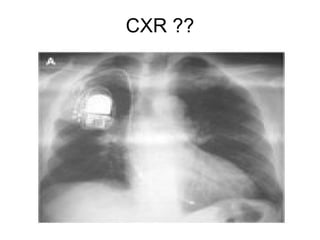
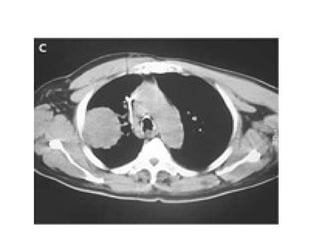
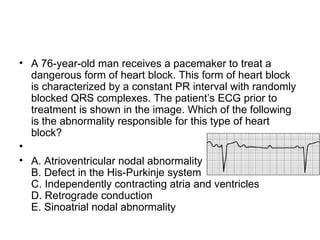
A 24-year-old man was hospitalized for evaluation of a dilated aorta and was diagnosed with Loeys-Dietz syndrome type 1 based on genetic analysis showing a mutation. An 83-year-old woman with atrial fibrillation and pacemaker presented with heart failure symptoms. Mortality rates after first hospitalization for heart failure are higher in men and increase with age.