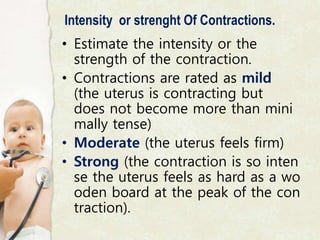
The document provides detailed information about the labor process, including fetal position, lie, attitude, and stages of labor. It describes the significance of fetal presentations, engagement, descent, and the physiological changes during labor, as well as signs of true and false labor. Additionally, it discusses the components and duration of normal labor along with methods for labor augmentation and the role of cervical effacement and dilation.