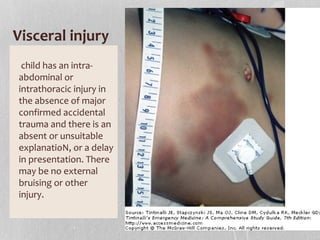
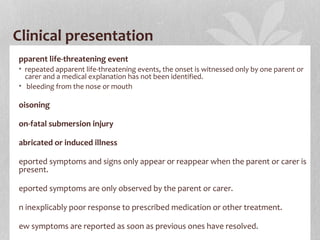
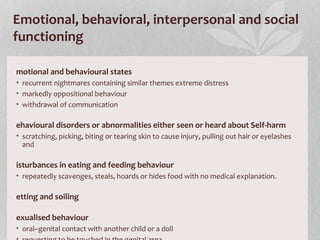
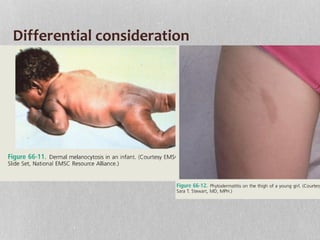
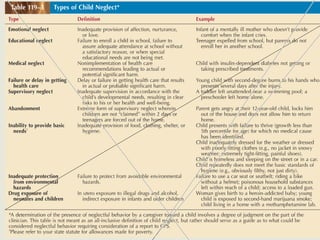
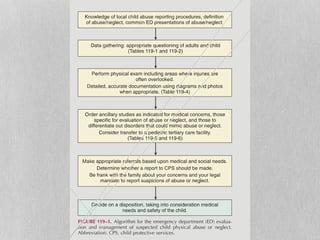
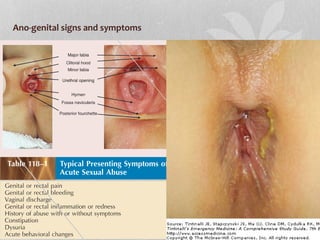
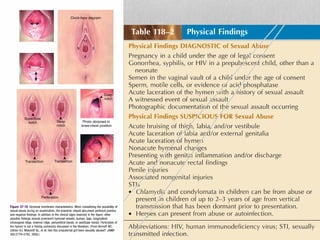
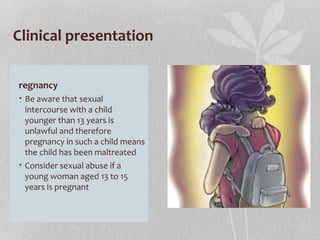
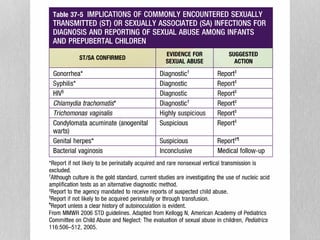
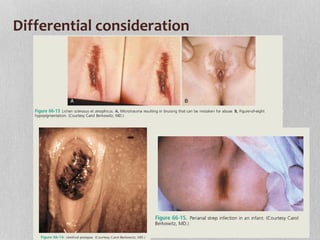
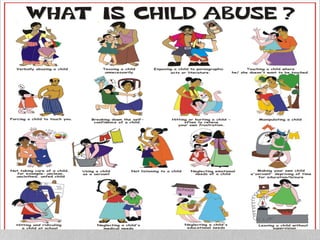
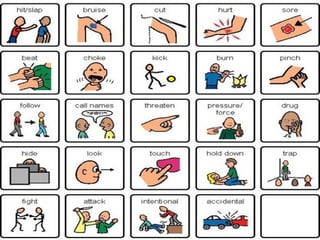
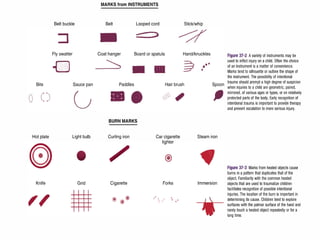
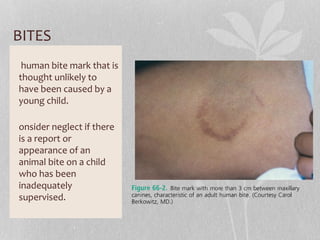
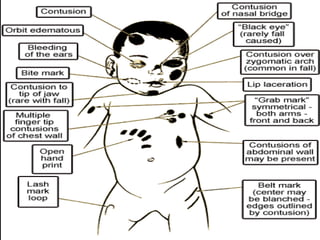
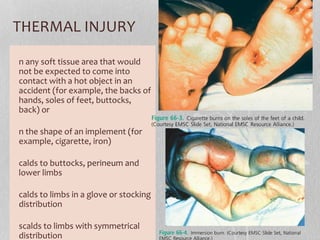
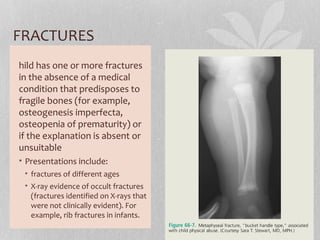
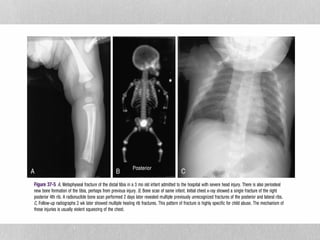
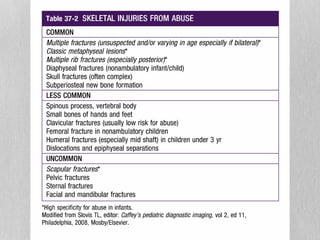
Physical abuse can be identified by bruises, bites, lacerations, burns, fractures, or intracranial injuries in locations not typical for accidental injury in children. Neglect can present as poor hygiene, malnutrition, or untreated medical issues. Sexual abuse may involve anogenital injuries, sexually transmitted infections, or pregnancy in young girls. Proper documentation and reporting to authorities is important for suspected cases of child abuse and neglect. A multidisciplinary approach is needed to manage cases and ensure children's safety and well-being.

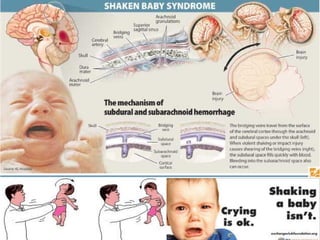
![INTRACRANIAL INJURY
bsence of major confirmed
accidental trauma or known medical
cause, in one or more of the
following circumstances:
he explanation is absent or
unsuitable[4] the child is aged under
3 years ,there are also:
• retinal haemorrhages or
• rib or long bone fractures or other
associated inflicted injuries
here are multiple subdural
haemorrhages with or without
subarachnoid haemorrhage with or
without hypoxic ischaemic damage
(damage due to lack of blood and
oxygen supply) to the brain.](https://image.slidesharecdn.com/childabuse-160204131209/85/Child-abuse-18-320.jpg)