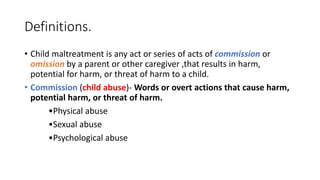
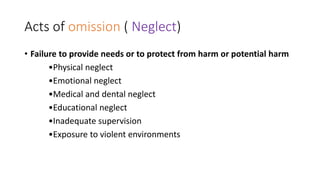
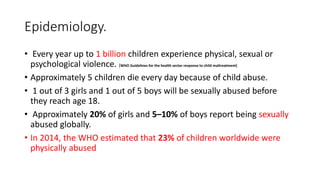
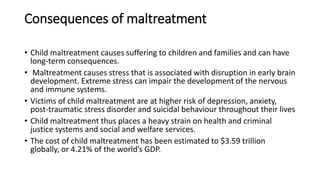
Child maltreatment is a significant global issue adversely affecting the physical and mental health of victims. It encompasses various forms of abuse and neglect, with millions of children experiencing violence each year, leading to profound long-term consequences. Factors contributing to maltreatment include personal caregiver characteristics, lack of resources, and excessive family stress, resulting in a heavy financial burden on health and social systems.