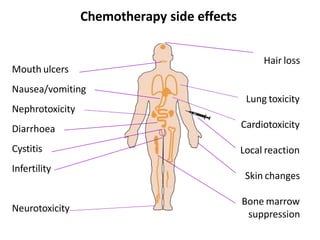
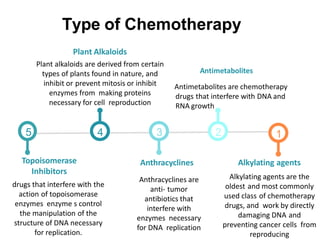
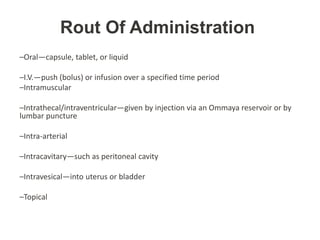
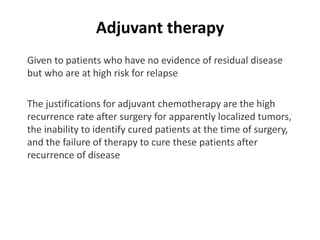
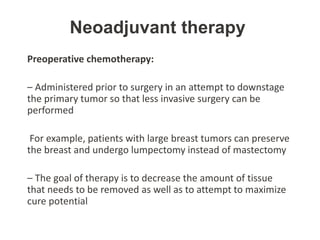
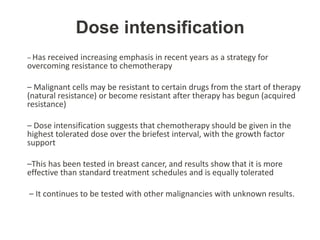
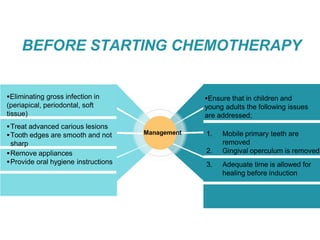
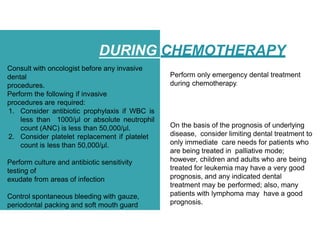
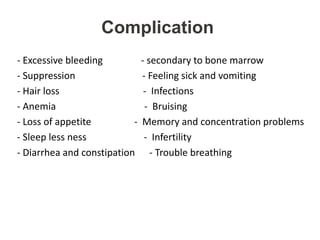
Chemotherapy is an aggressive form of treatment that uses chemical drugs to destroy rapidly growing cancer cells. It works by damaging the DNA of active cells, including both cancer and healthy cells, which causes common side effects. The goals of chemotherapy are to eliminate cancer, shrink tumors, prevent the spread of cancer, and relieve symptoms. There are several types of chemotherapy drugs that work through different mechanisms. Chemotherapy is usually administered through oral, intravenous, intramuscular, or other routes of administration. Adjuvant and neoadjuvant chemotherapy are given before or after other treatments. High dose chemotherapy aims to overcome drug resistance. Oral health management before, during, and after chemotherapy is important to prevent infections and complications.