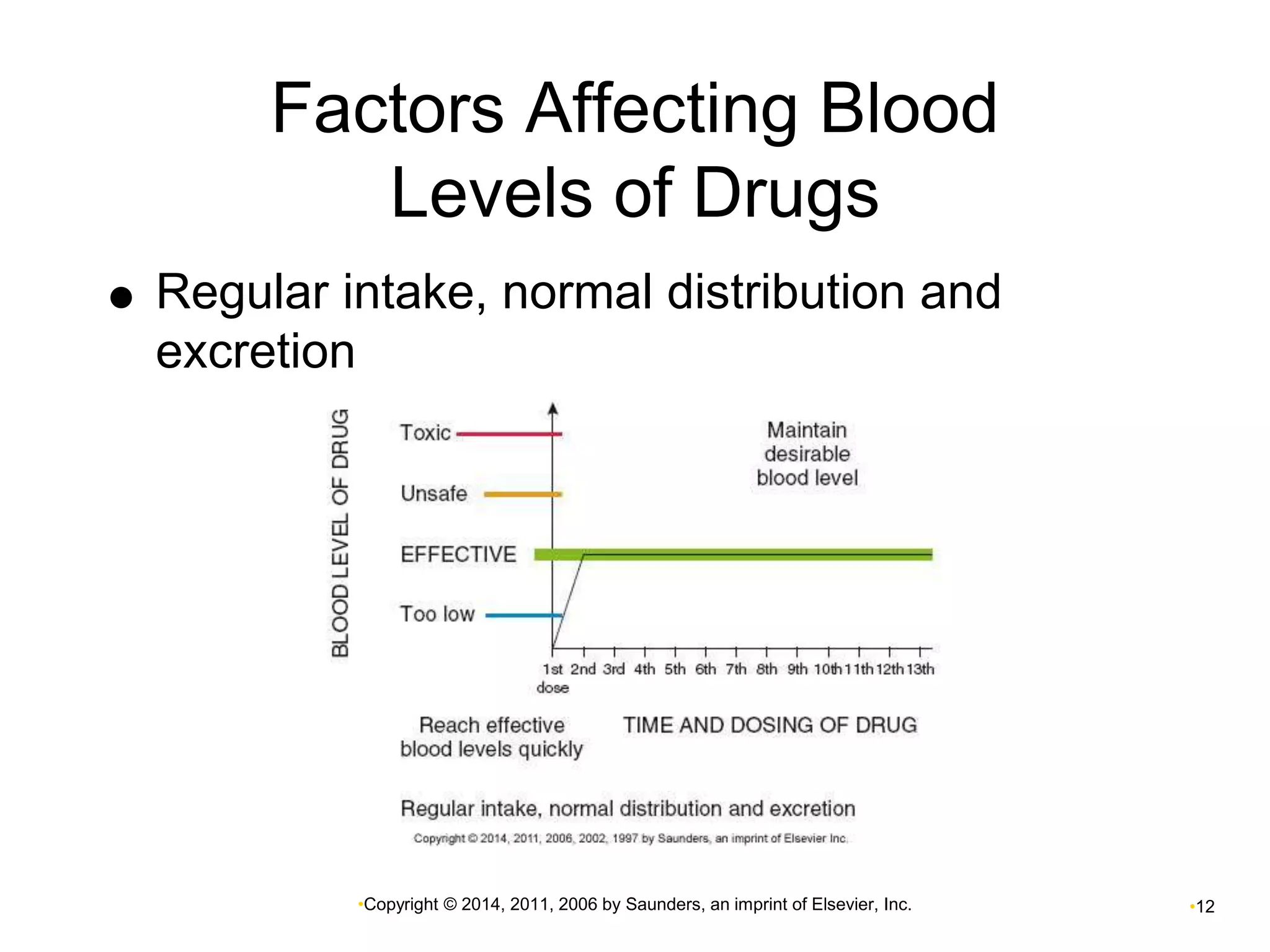
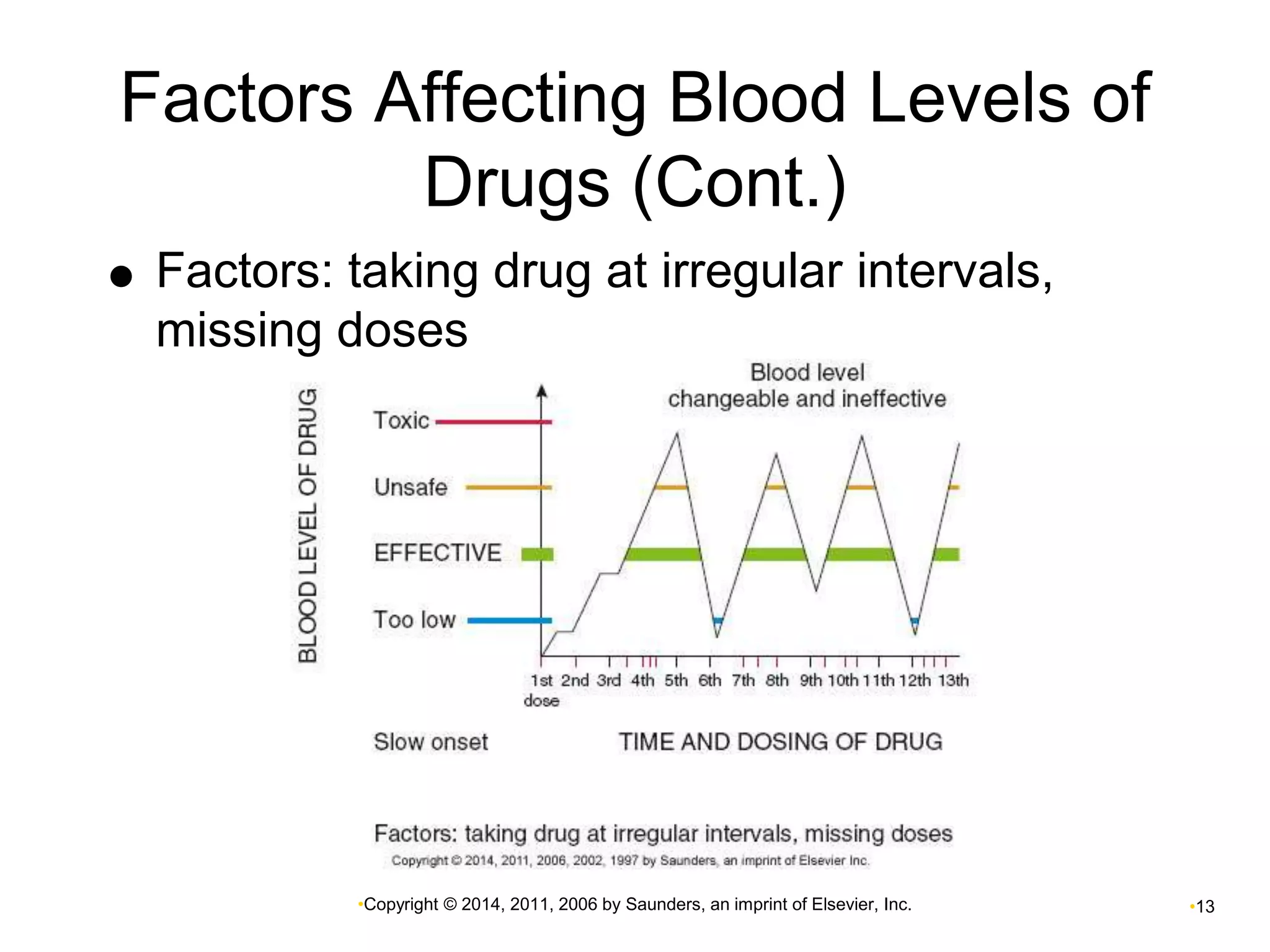
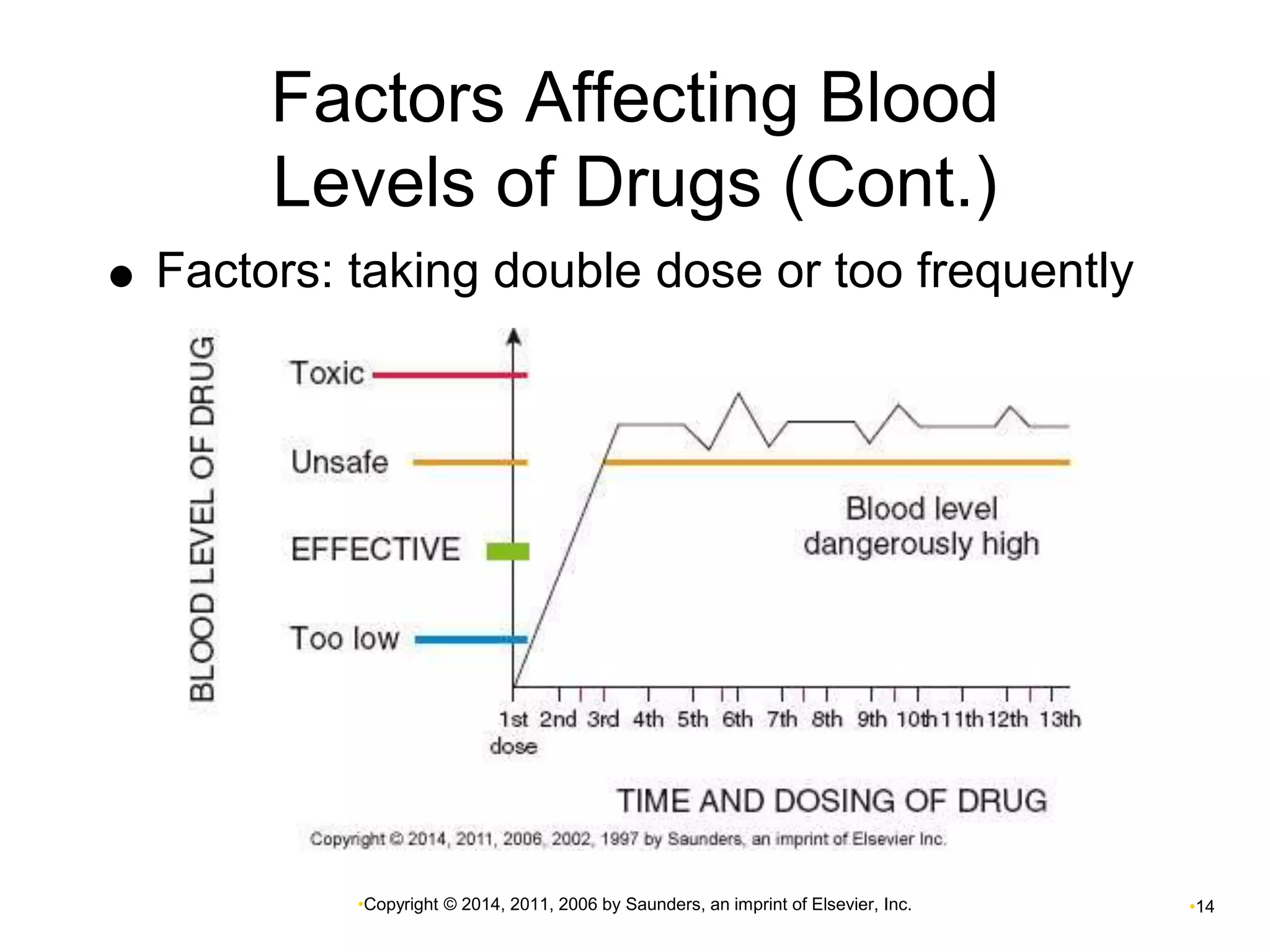
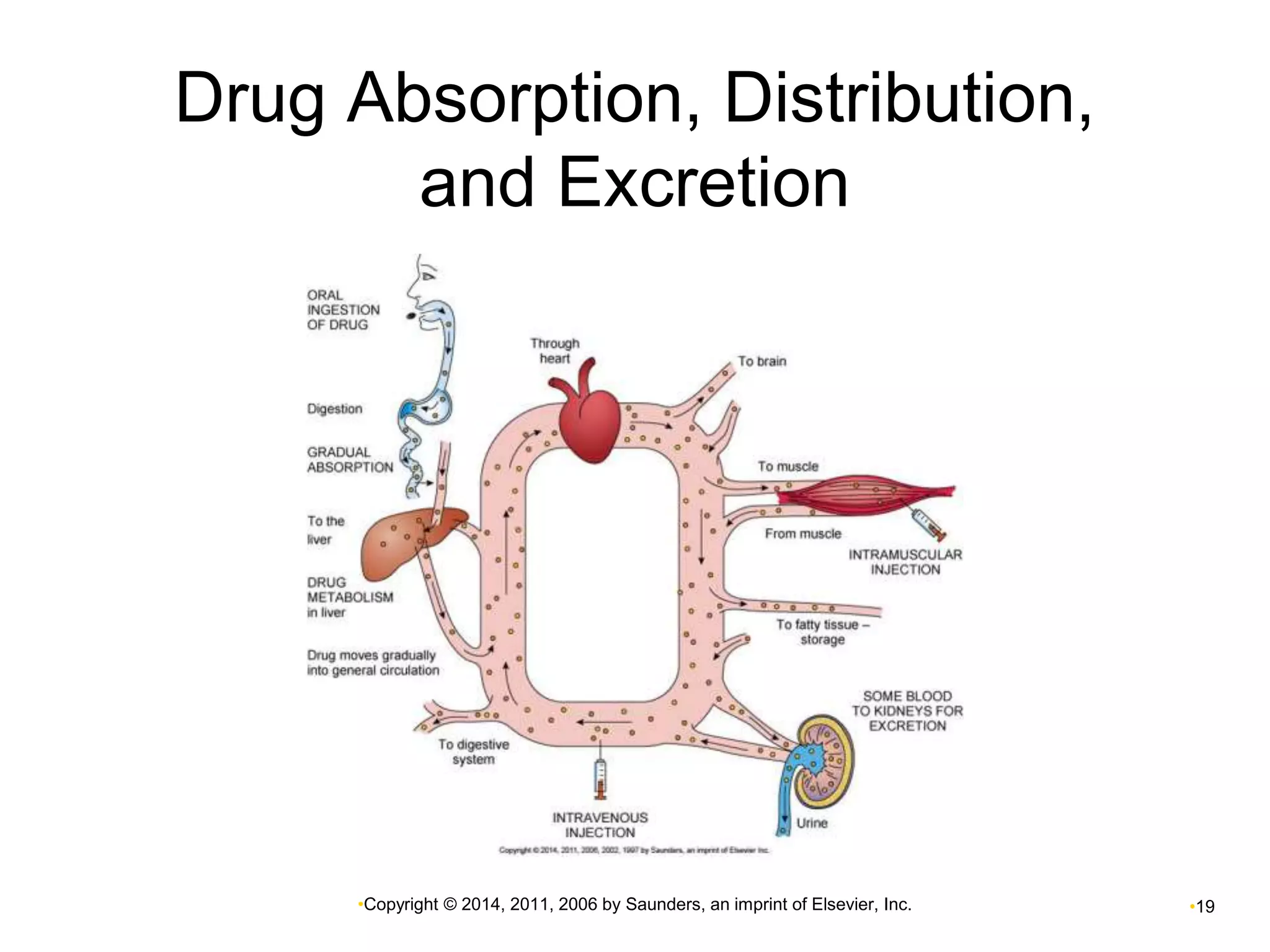
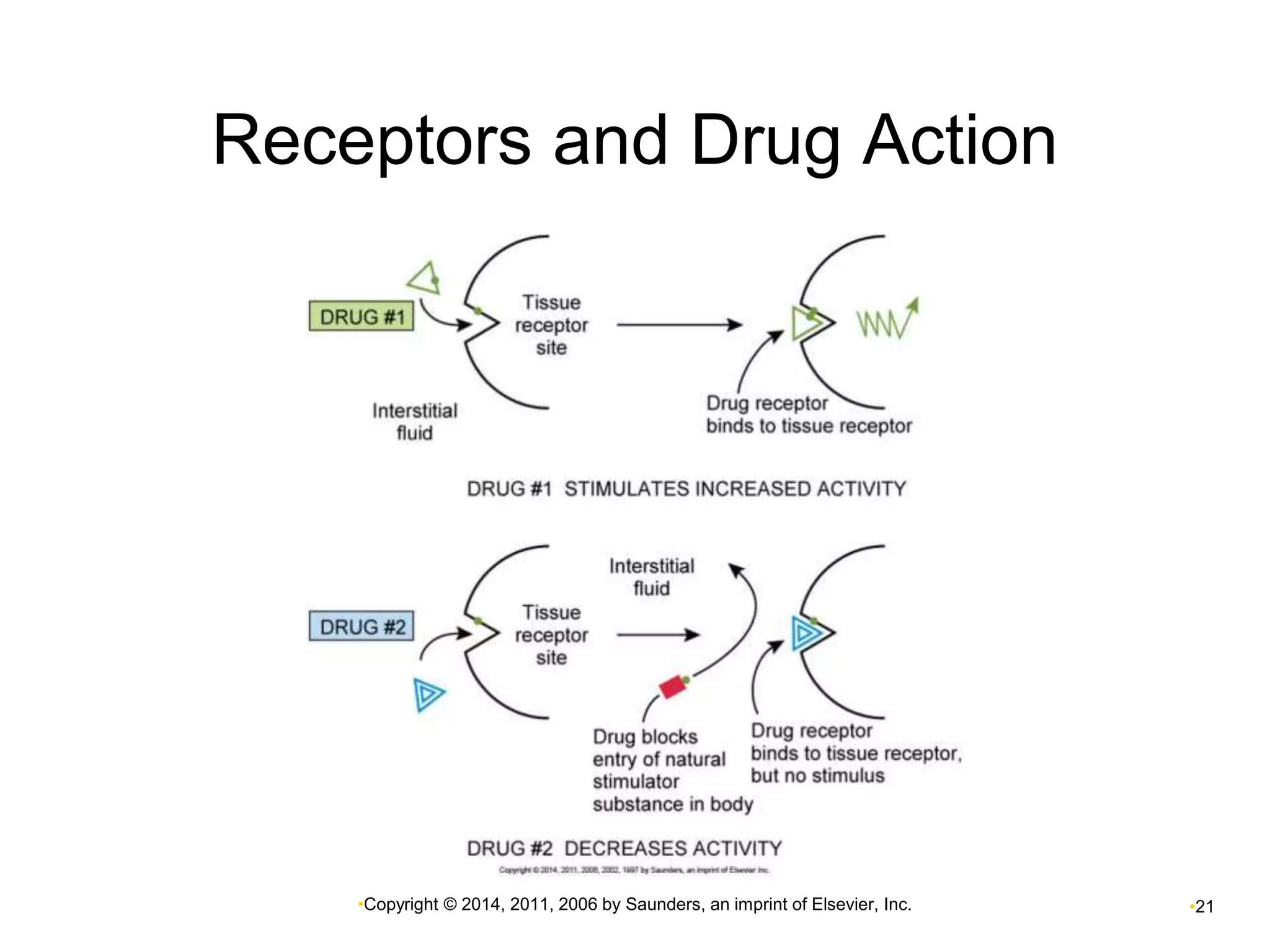
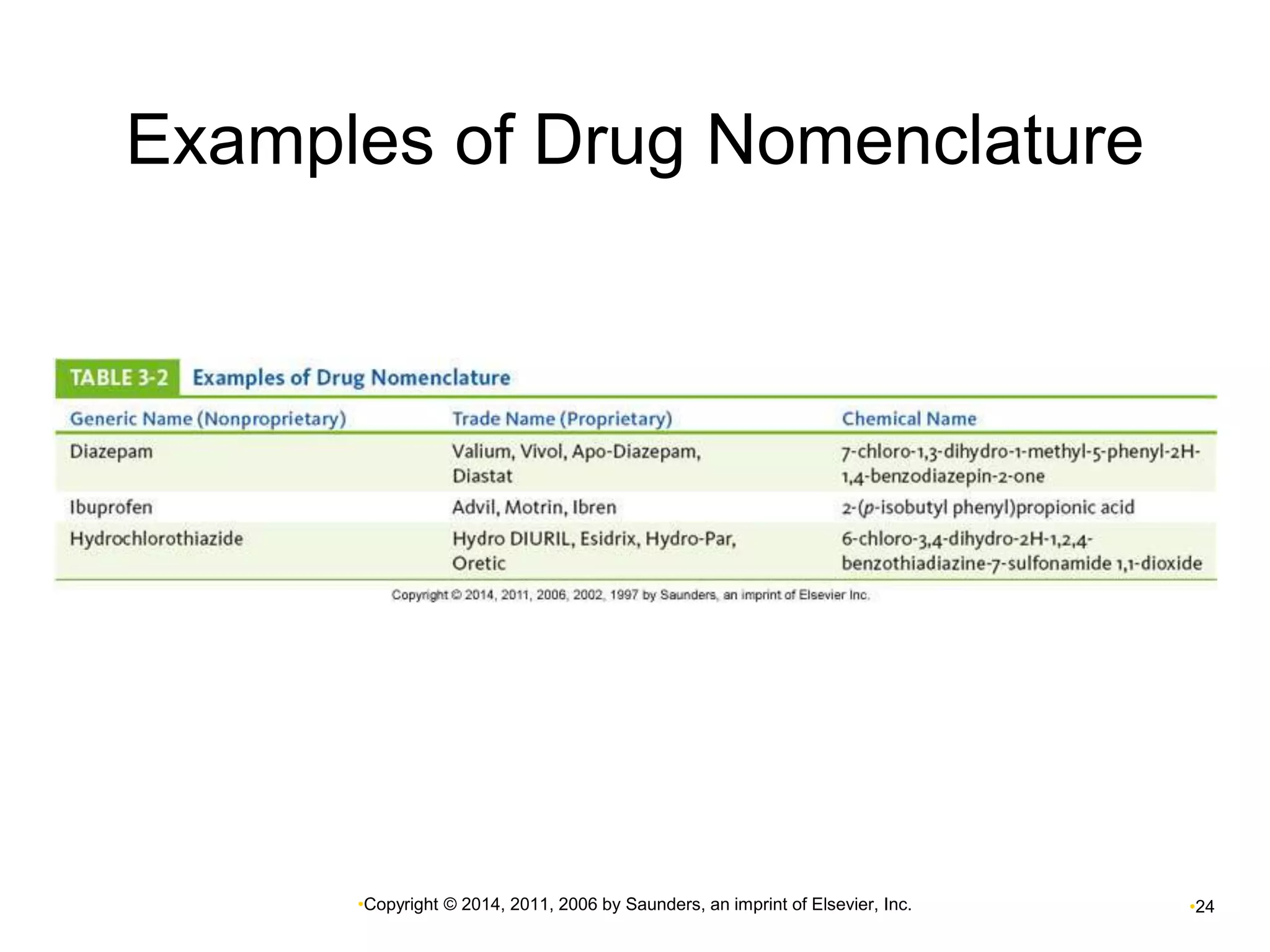
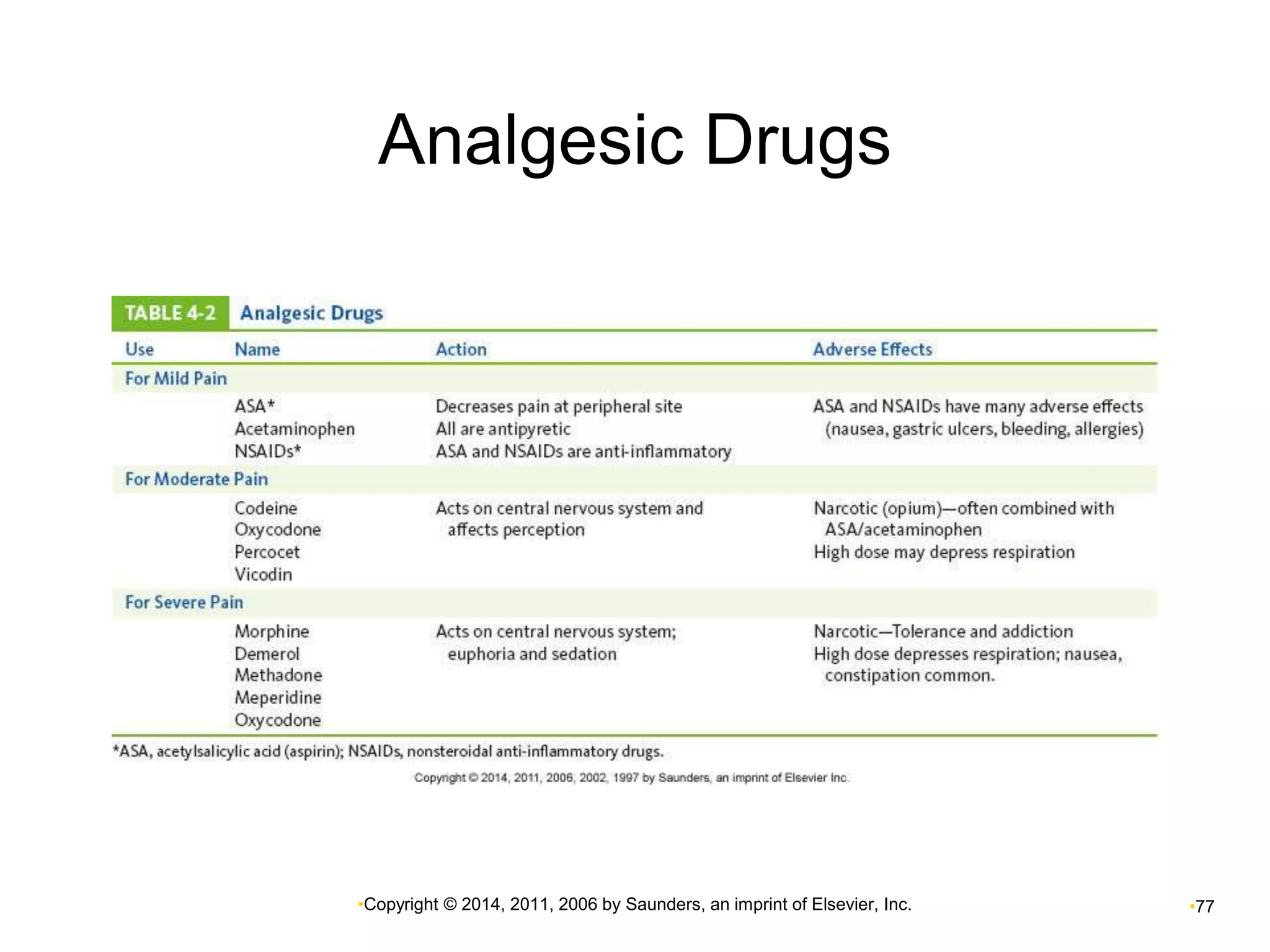
This document provides an overview of pharmacology and common medical therapies. It defines pharmacology and describes how drugs can be used to treat diseases, relieve symptoms, and replace deficient hormones or enzymes. Various drug administration routes, mechanisms of action, and factors influencing drug effects are examined. Common medical therapies including physiotherapy, occupational therapy, nutrition, and complementary/alternative approaches like herbalism and aromatherapy are also summarized.