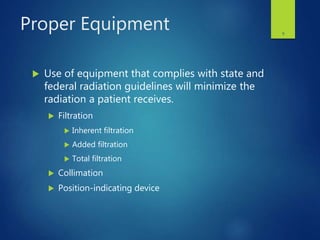
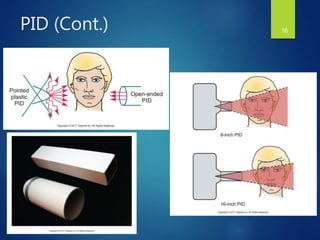
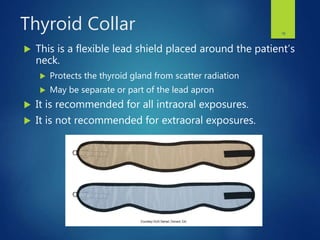
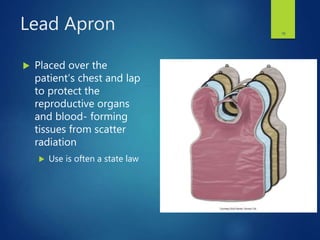
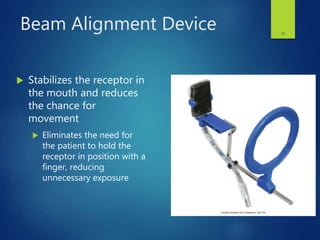
This document discusses radiation protection for patients and operators during dental x-ray procedures. It covers key concepts like total filtration, collimation, protective equipment like lead aprons and thyroid collars, proper techniques to minimize exposure, and guidelines for radiation safety. The document emphasizes that while dental x-rays provide benefits, it is important to use all available methods to minimize the amount of radiation received by patients and operators, in accordance with legislation and the ALARA principle of keeping exposures as low as reasonably achievable.