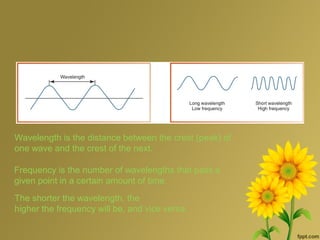
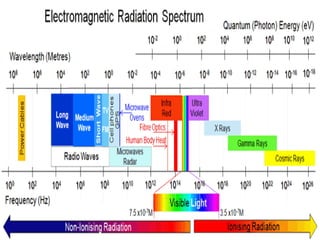
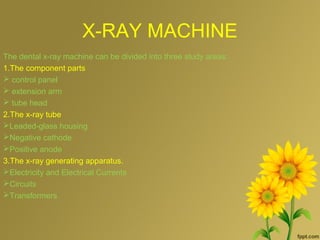
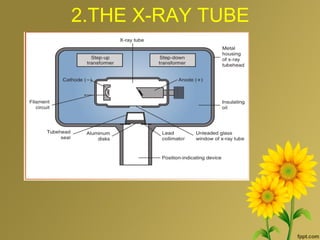
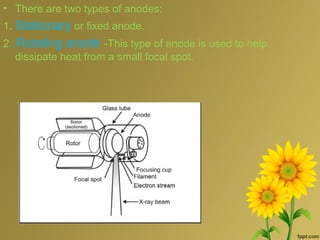
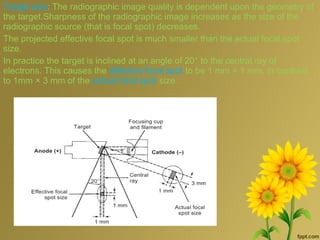
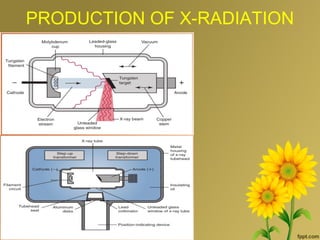
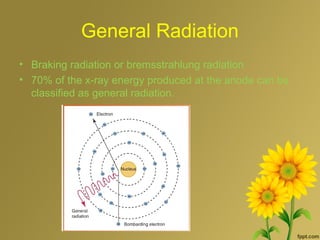
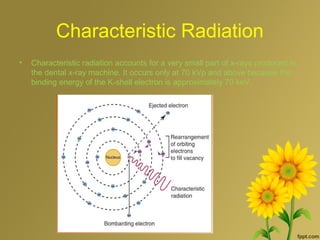
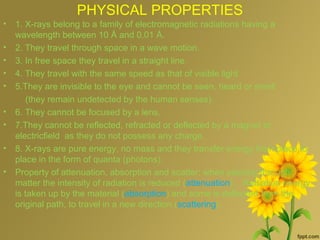
This document provides information about x-rays and x-ray machines. It discusses the production of x-radiation through both braking radiation and characteristic radiation. The properties of x-rays include their physical properties like wavelength and speed of travel, as well as their ability to ionize atoms. The document also describes the components of an x-ray machine including the cathode, anode, collimator and transformers used to generate x-rays.