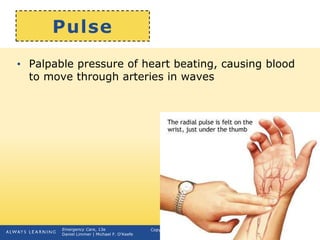
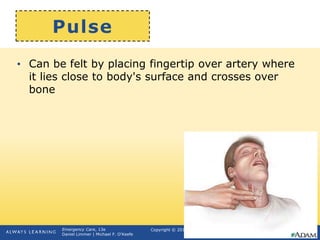
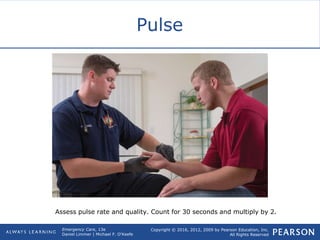
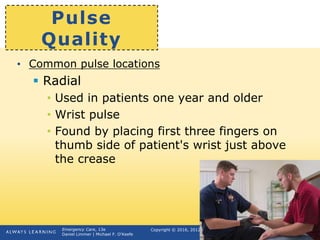
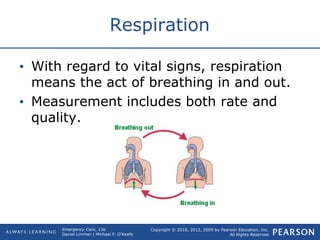
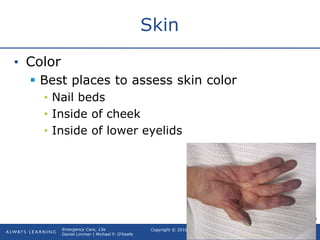
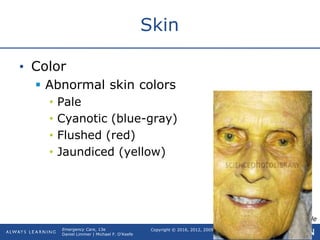
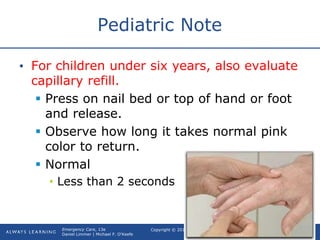
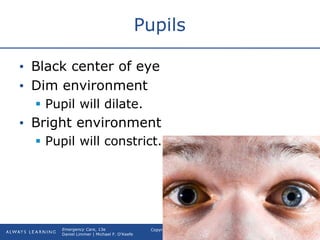
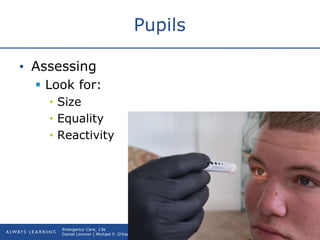
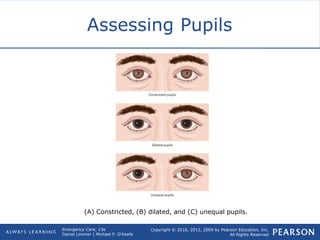
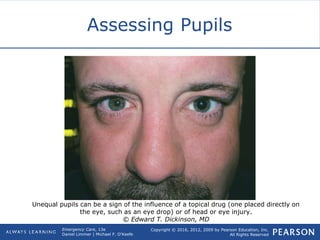
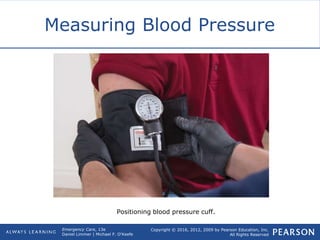
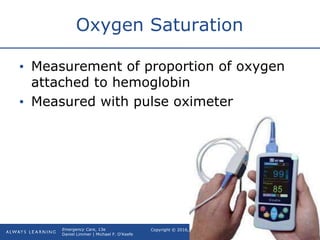
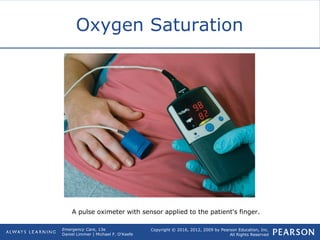
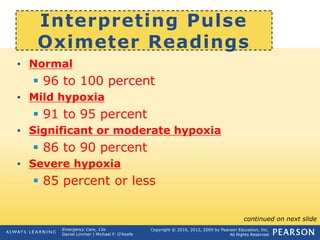
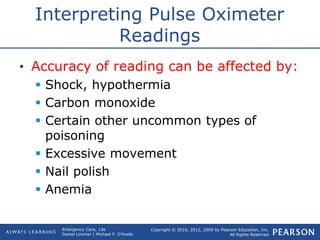
This document provides an overview of how to gather and assess vital signs, including pulse, respiration, skin, pupils, and blood pressure. It describes the normal ranges for adults and how to monitor each vital sign by counting rates, evaluating rhythms and qualities, and identifying abnormal findings that may require further attention. Vital signs are important for identifying a patient's condition and monitoring changes over time during emergency medical care.