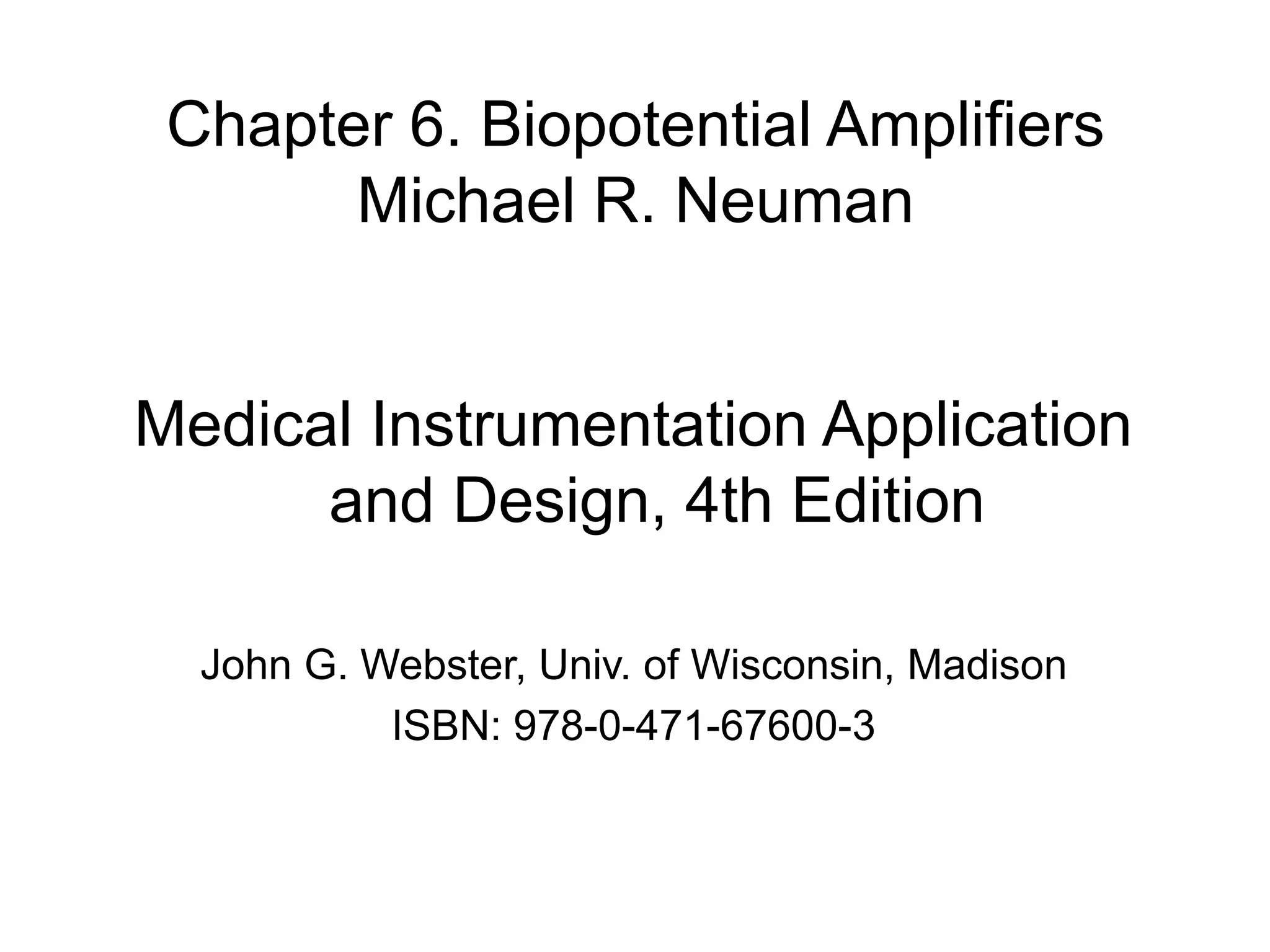
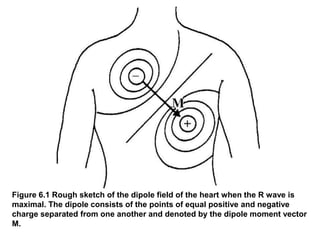
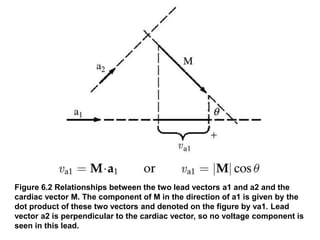
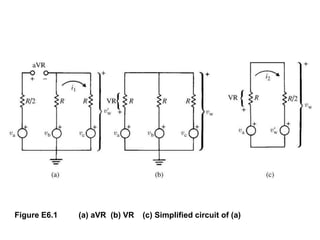
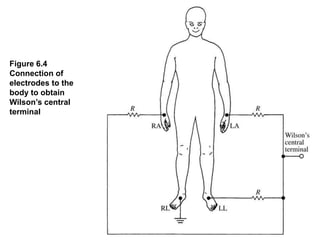
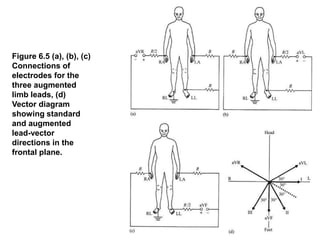
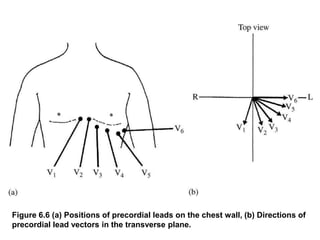
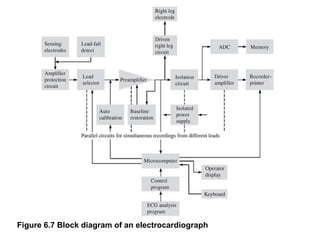
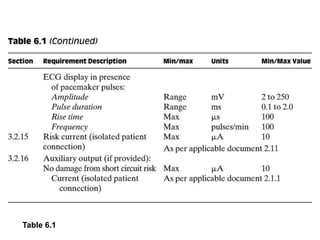
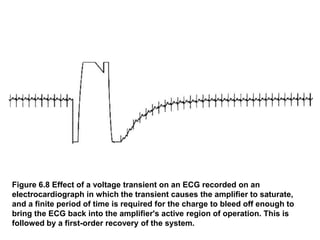
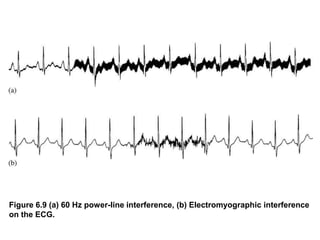
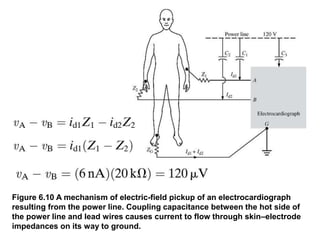
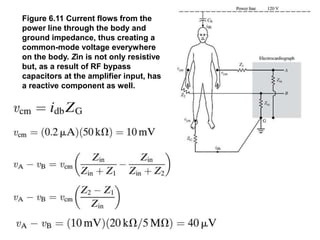
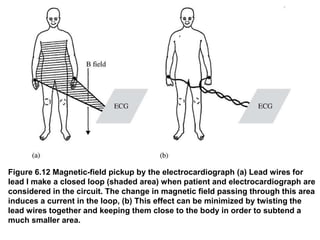
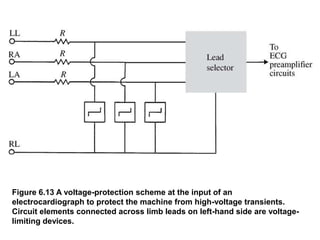
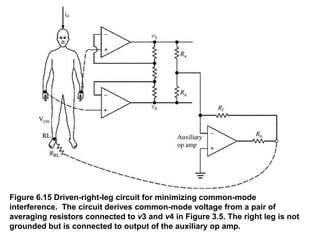
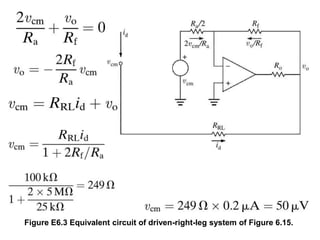
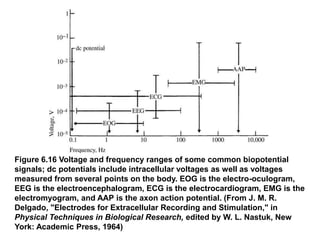
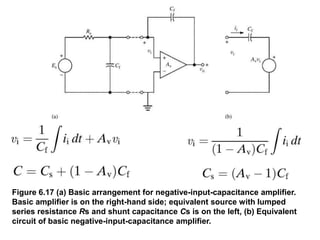
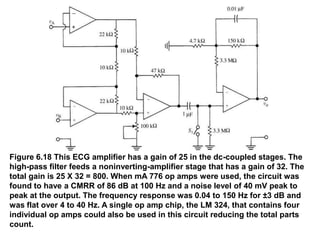
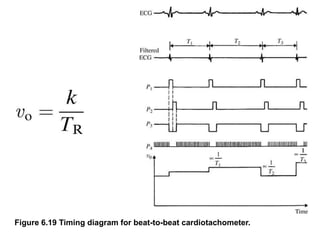
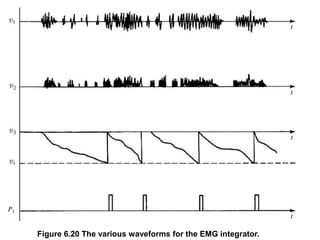
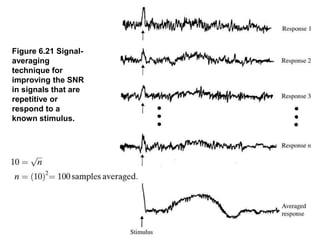
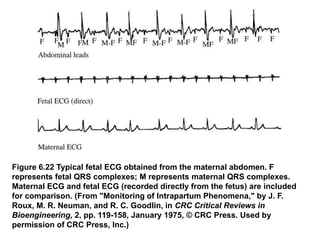
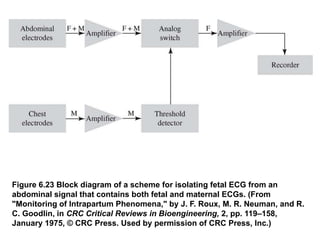
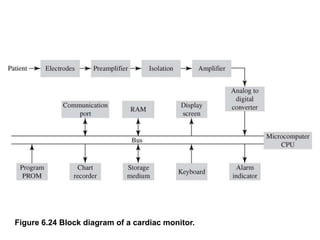
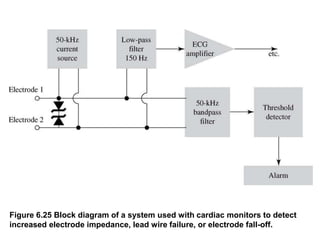
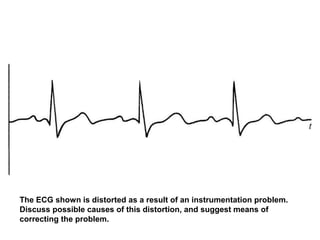
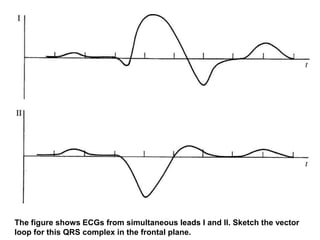
This document discusses biopotential amplifiers used in medical instrumentation to measure weak bioelectric signals such as electrocardiograms (ECGs). It includes figures illustrating cardiac vector loops, lead connections, sources of noise and interference, circuit diagrams for amplifier designs, and applications like fetal monitoring. Protection circuits and filtering techniques are presented to improve signal quality and reduce noise from sources like power lines and muscle activity.