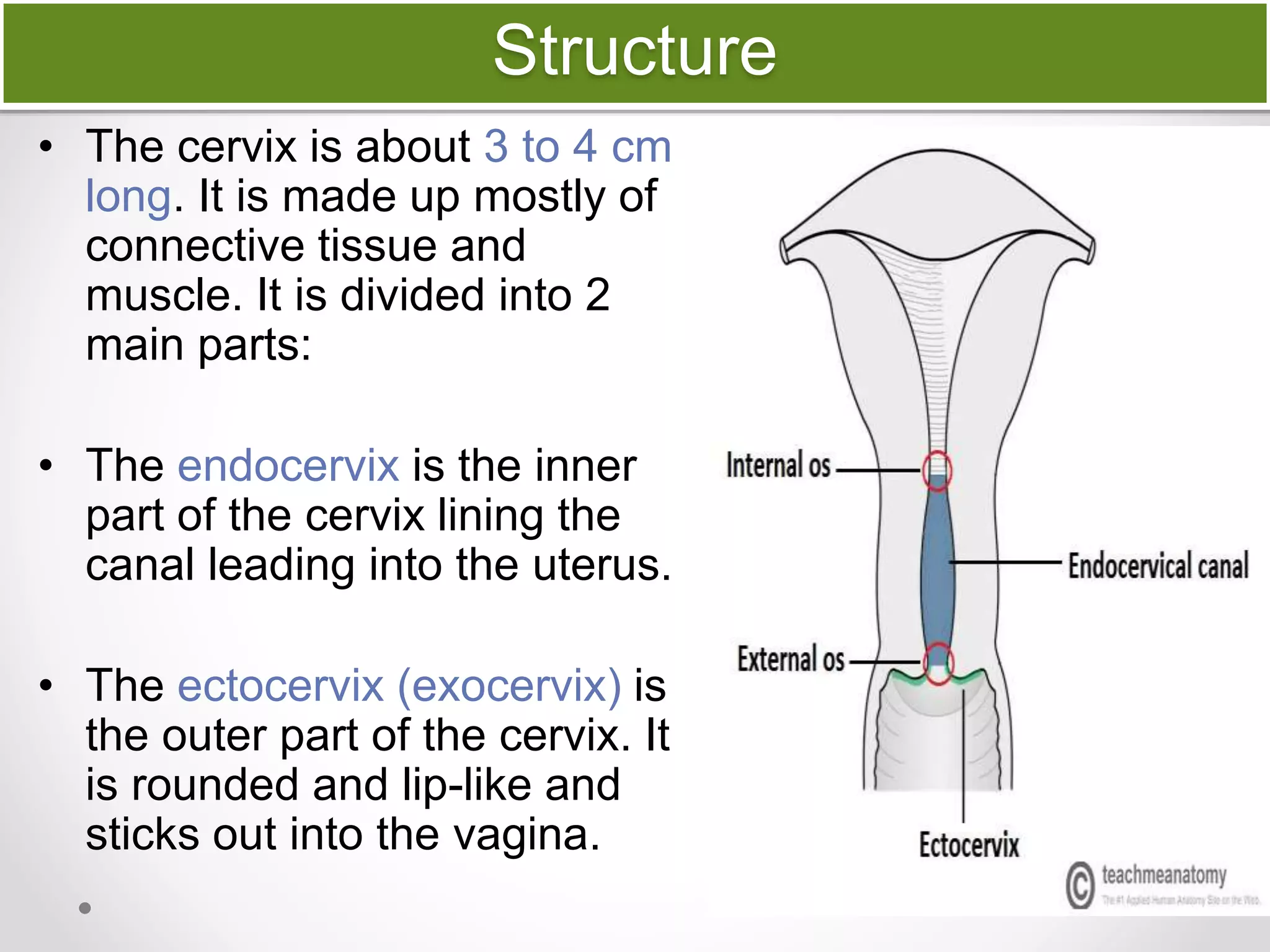
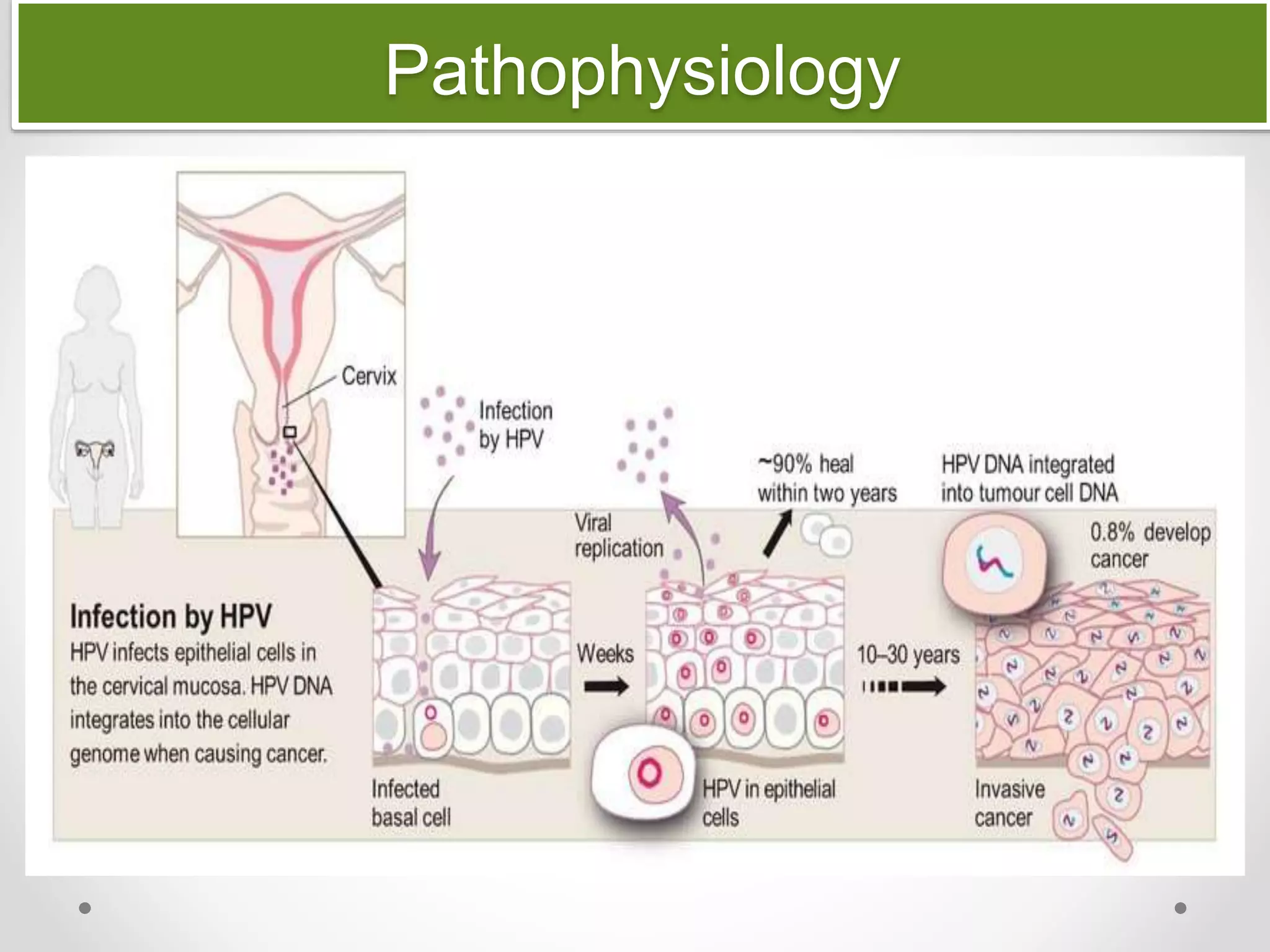
Annie is a 45-year-old divorced mother who has had multiple sexual partners. She was treated for genital warts last year and her recent Pap smear showed abnormal cells. Cervical cancer develops from pre-cancerous changes to the cervix over time. Persistent HPV infection is the main risk factor. Early screening allows detection before symptoms occur and treatment can be effective.