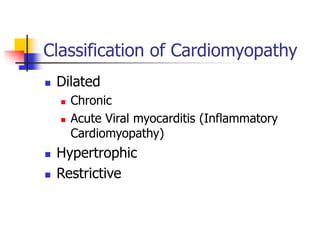
This document discusses cardiomyopathy in neonates and children. It covers the classification, epidemiology, causes, pathophysiology, clinical presentation, diagnostic evaluation, and management of various types of cardiomyopathy including dilated, hypertrophic, restrictive, and ischemic cardiomyopathy. The key points are:
1. Cardiomyopathy can present as recurrent wheezing in children and has an incidence of 1 in 100,000 with higher rates in infancy. Common causes include viral myocarditis, genetic factors, and metabolic disorders.
2. Diagnostic evaluation involves ECG, echocardiogram, blood tests, and cardiac catheterization. Echocardiogram can identify features like ventricular dilation or hypertrophy