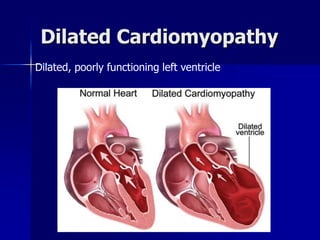
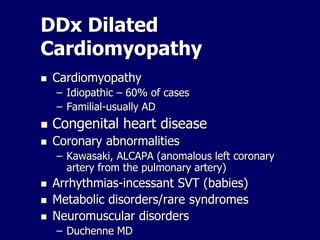
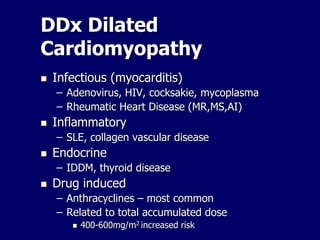
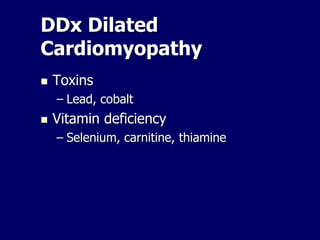
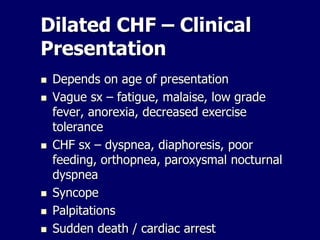
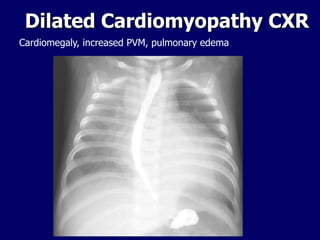
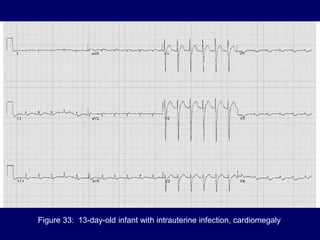
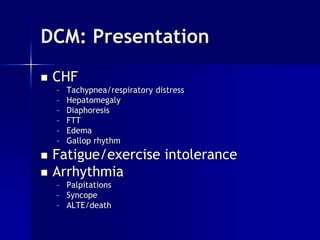
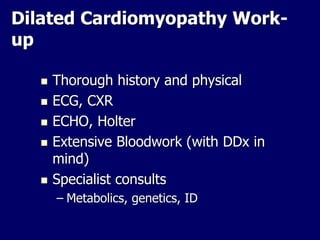
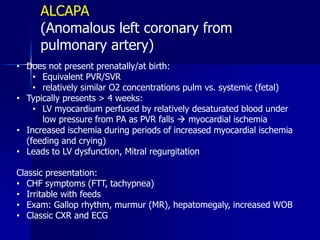
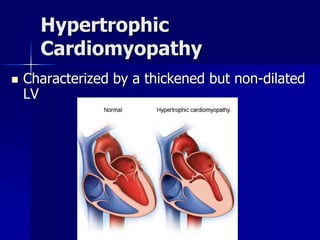
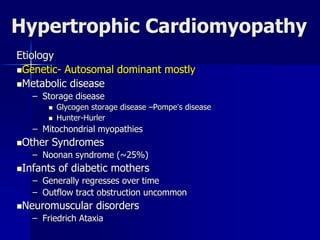
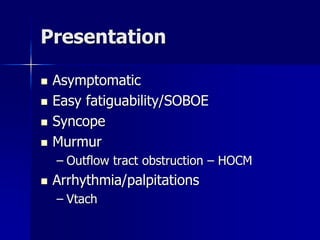
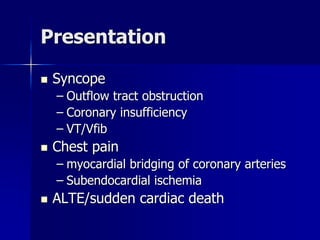
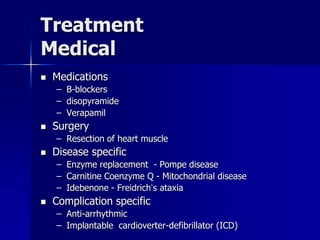
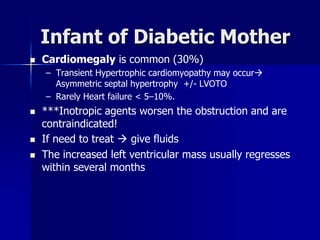
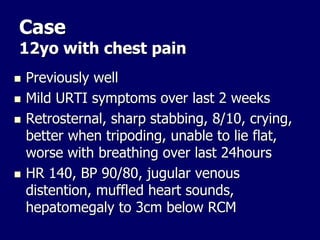
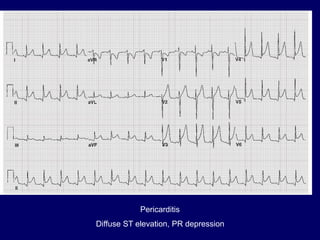
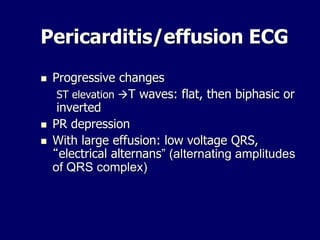
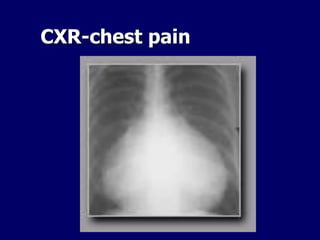
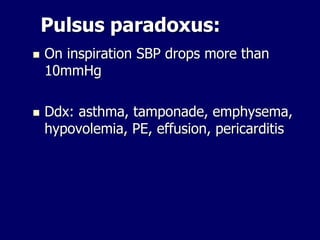
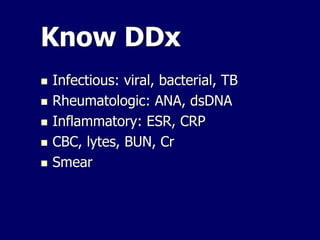
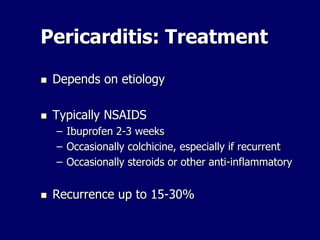
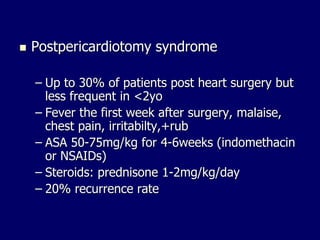
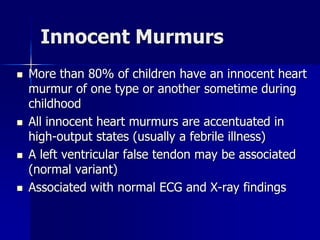
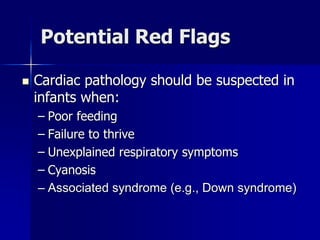
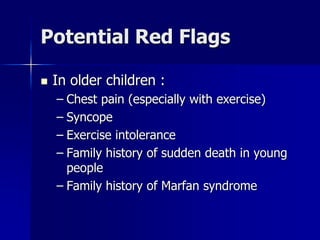
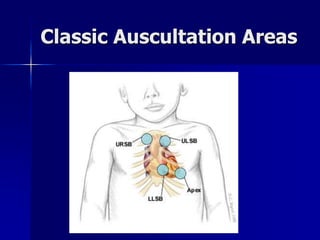
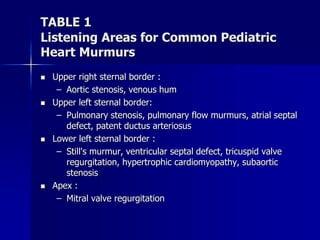
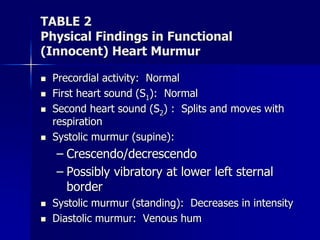
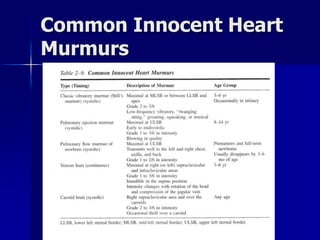
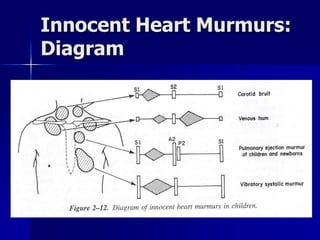
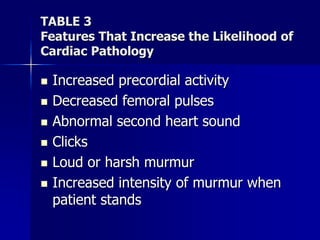
This document discusses various cardiomyopathies including dilated, hypertrophic, and restrictive cardiomyopathies. It provides details on dilated cardiomyopathy including causes, clinical presentation, workup, and management. Hypertrophic cardiomyopathy etiology, presentation, and treatment are summarized. The document also reviews pericarditis including presentation, ECG and imaging findings, differential diagnosis, and treatment. Common pediatric heart murmurs and features that suggest an innocent murmur versus potential cardiac pathology are presented.