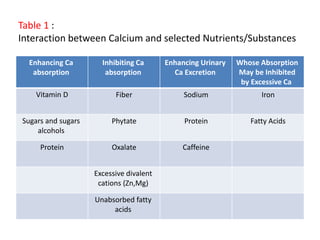
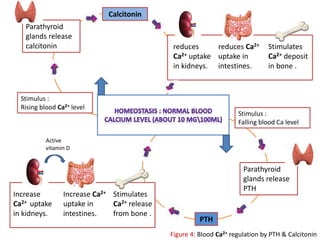
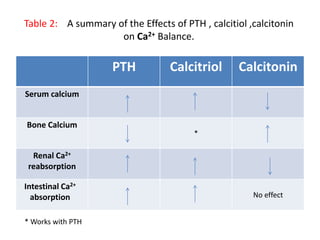
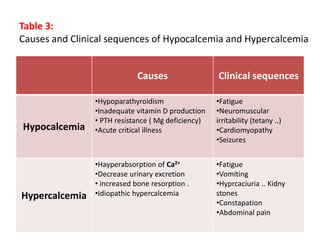
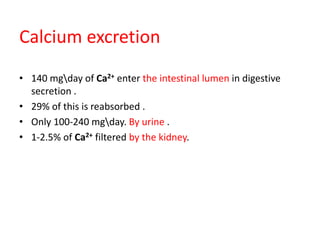
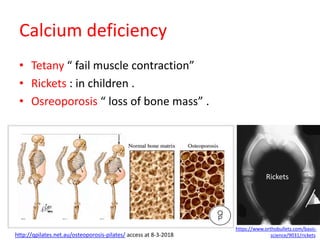
The document provides an overview of calcium as an essential mineral in human nutrition, detailing its properties, sources, absorption mechanisms, and physiological roles such as bone mineralization, nerve conduction, and blood coagulation. It discusses the regulation of calcium homeostasis through hormones like parathyroid hormone and calcitonin, and highlights the consequences of calcium deficiency and excess. Additionally, it mentions the recommended daily intake and the impact of dietary factors on calcium bioavailability.


![2- Paracellular transport :
occurs between cells The process allows the movement
(Diffusion) of Ca .
Occurs when :
- High [ Ca ] in lumen.
- Gradient of [ Ca ] between the lumen and basoletral side .](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-8-320.jpg)





![3 types of bone cells :
• Osteoblast :
- called (Bone building cells)
- Produce matrix
- secret collagen and ground substance .
- become ostocytes .
• Osteocytes :
- Star shaped
- mature bone cells
• Osteoclasts :
- Phagocytic cell
-role in increasing blood [Ca2+ ]
-contain lysosomes and enzymes capable of breaking down.](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-18-320.jpg)









![Blood
Low [Ca]
Gastrointestinal
Tract
Basolate
membrane
Brush border
membrane
Calcitriol
Ca2+
Figure 5: Blood Ca2+ regulation by calcitriol in response to low blood [Ca2+ ] .](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-30-320.jpg)

![:Figure 5
Regulation of intracellular [calcium]](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-33-320.jpg)
![Lower [Ca2+ ] By
• Buffering free Ca2+ via molecular sequestration.
• compartmentalization* of Ca2+ through uptake in to cellular
organells.
• Removal of excess Ca2+ from the cell via energy-dependent Ca2+
pumps found on Plasma membrane.
* compartmentalize meaning : to separate something into parts and
not allow those parts to mix together.
Removal of Ca2+ stimulus](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-34-320.jpg)



![Assessment
• Difficult to assess : same indicators of Vitamin D
status , bone disease , hormonal imbalance.
methods :
• presence of normal [albumin]
• CT scans
• DEXA : the best “ change in mass over time”](https://image.slidesharecdn.com/calcium-180421211800/85/Calcium-42-320.jpg)