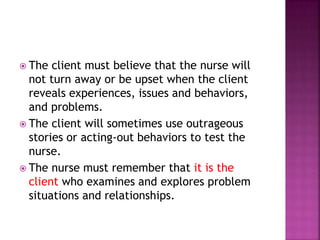
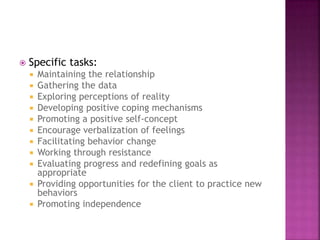
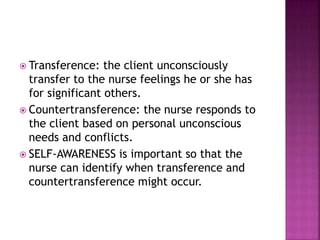
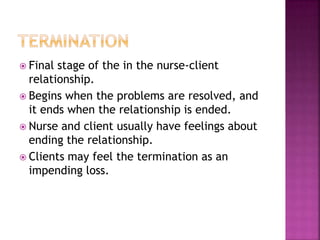
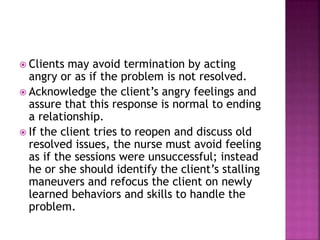
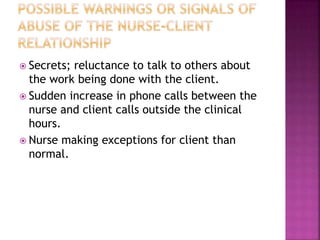
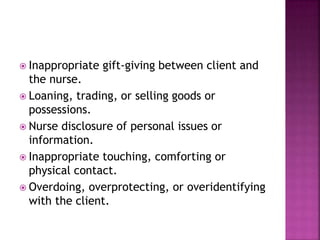
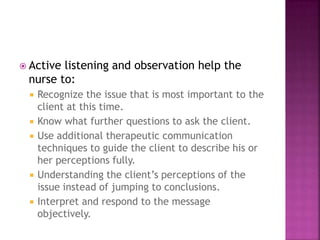
The document discusses various types of relationships in nursing, including social, intimate, therapeutic, and transference relationships. It emphasizes that the nurse-client relationship must remain strictly professional and focused on the client's needs. The nurse must establish trust and set clear boundaries to avoid relationships becoming social or intimate. The stages of a therapeutic relationship are explored, including engagement, assessment, intervention, and termination. Factors that can threaten appropriate boundaries are also outlined.