Embed presentation
Downloaded 11 times
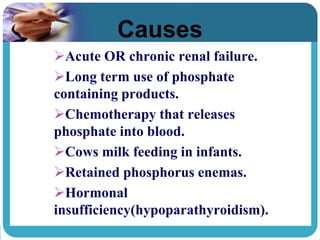
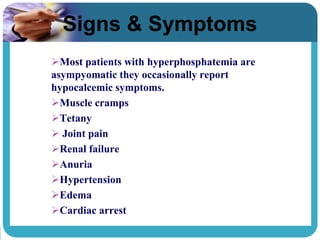
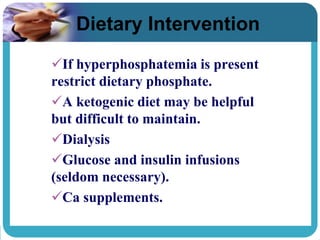
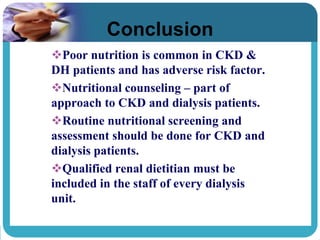

Hyperphosphatemia is a condition where there are abnormally high levels of phosphate in the blood. It is commonly caused by chronic kidney disease and can lead to morbidity and mortality. Symptoms may include muscle cramps, tetany, and joint pain. Dietary interventions to treat hyperphosphatemia include restricting phosphate intake and following a ketogenic diet. Nutritional counseling and dietary assessments by a renal dietitian are important for managing the condition in patients with chronic kidney disease or on dialysis.