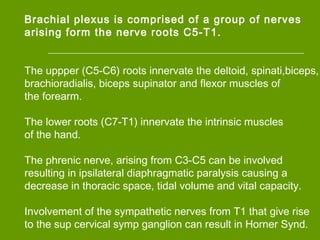
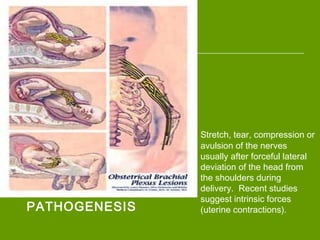
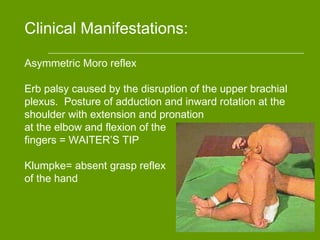
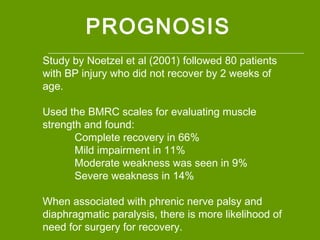
This document summarizes brachial plexus injuries in neonates. It discusses the epidemiology, anatomy, pathogenesis, clinical manifestations, diagnostic workup, management, prognosis, and references for brachial plexus injuries. Brachial plexus injuries affect 0.5-1.9 per 1000 live births and are most commonly caused by shoulder dystocia during delivery, stretching and damaging the brachial plexus nerves. Clinical signs depend on the specific nerves injured but may include limited arm movement and hand grasp. Management involves initial rest and positioning of the infant, with potential later surgery and physical therapy if nerve damage does not improve on its own. Prognosis is generally good, with most infants recovering fully or with