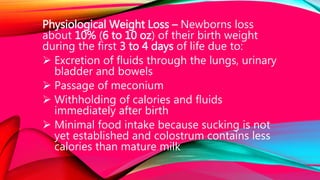
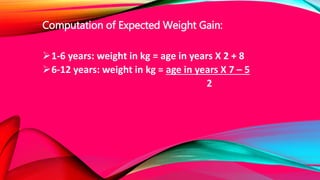
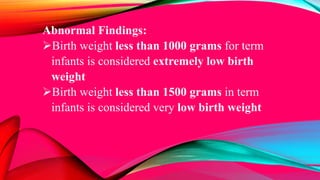
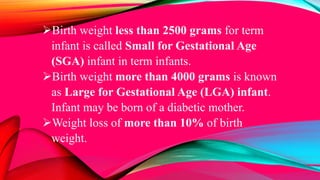
The document outlines critical measurements of infants including head circumference (HC), chest circumference (CC), abdominal circumference (AC), weight, and length, detailing normal ranges, measurement techniques, and implications of abnormal findings. It emphasizes the importance of monitoring these parameters for assessing newborn health and growth, as well as potential complications such as microcephaly or hydrocephalus. Additionally, it discusses physiological changes, weight gain patterns, and the significance of taking accurate measurements for better clinical outcomes.









































































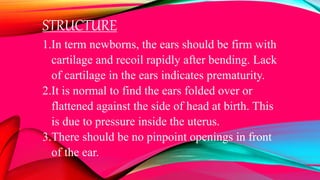
![4. Otoscopic examination is not advisable in
newborns because the ear canal is usually filled
with amniotic fluid that interferes with
visualization of the tympanic membrane.
5. Ears are considered small if less than 2.5 cm
[5] in the term neonate.](https://image.slidesharecdn.com/importantmeasurements-mid102-140825025254-phpapp01/85/Important-measurements-of-a-newborn-100-320.jpg)