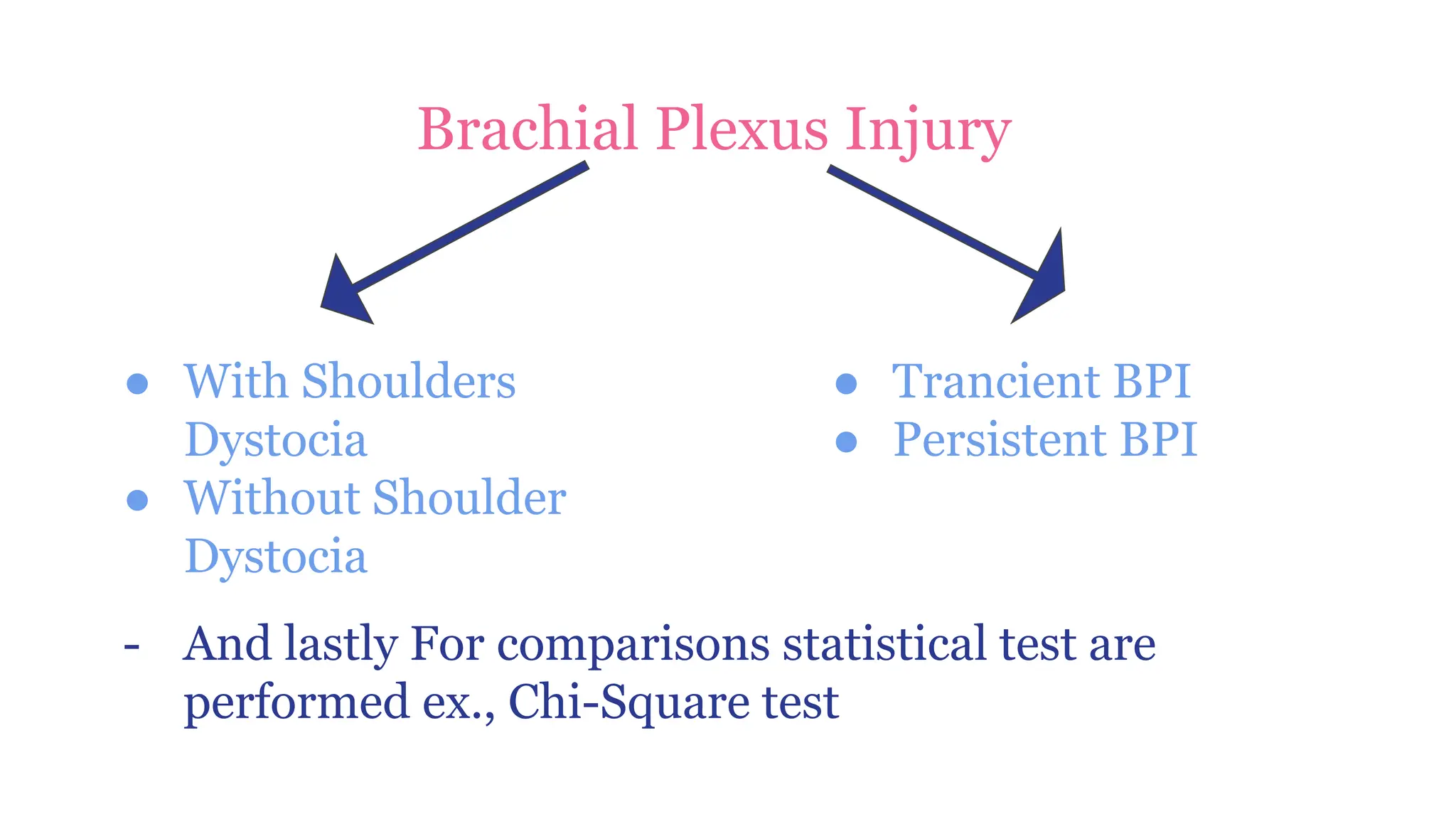
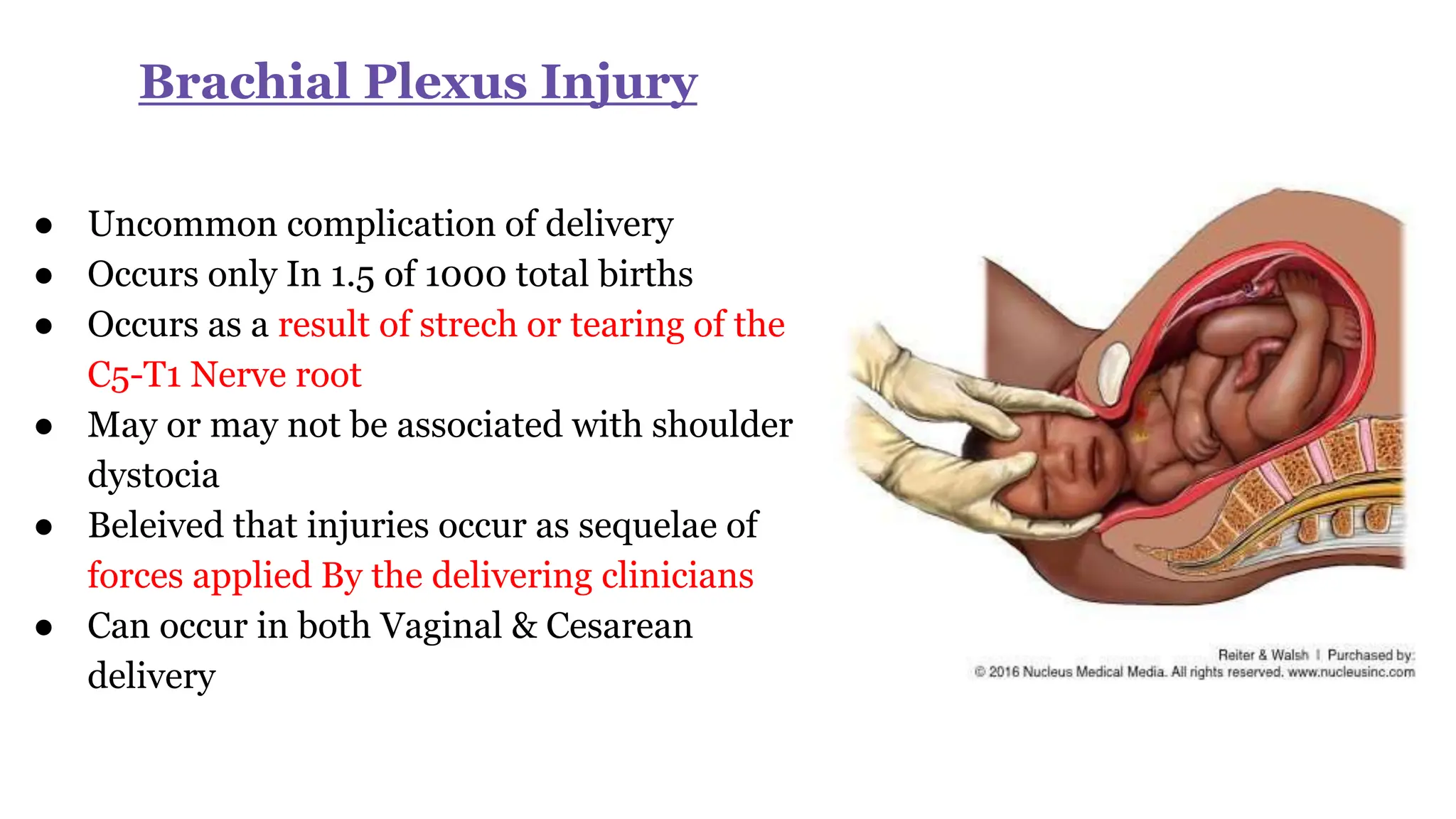
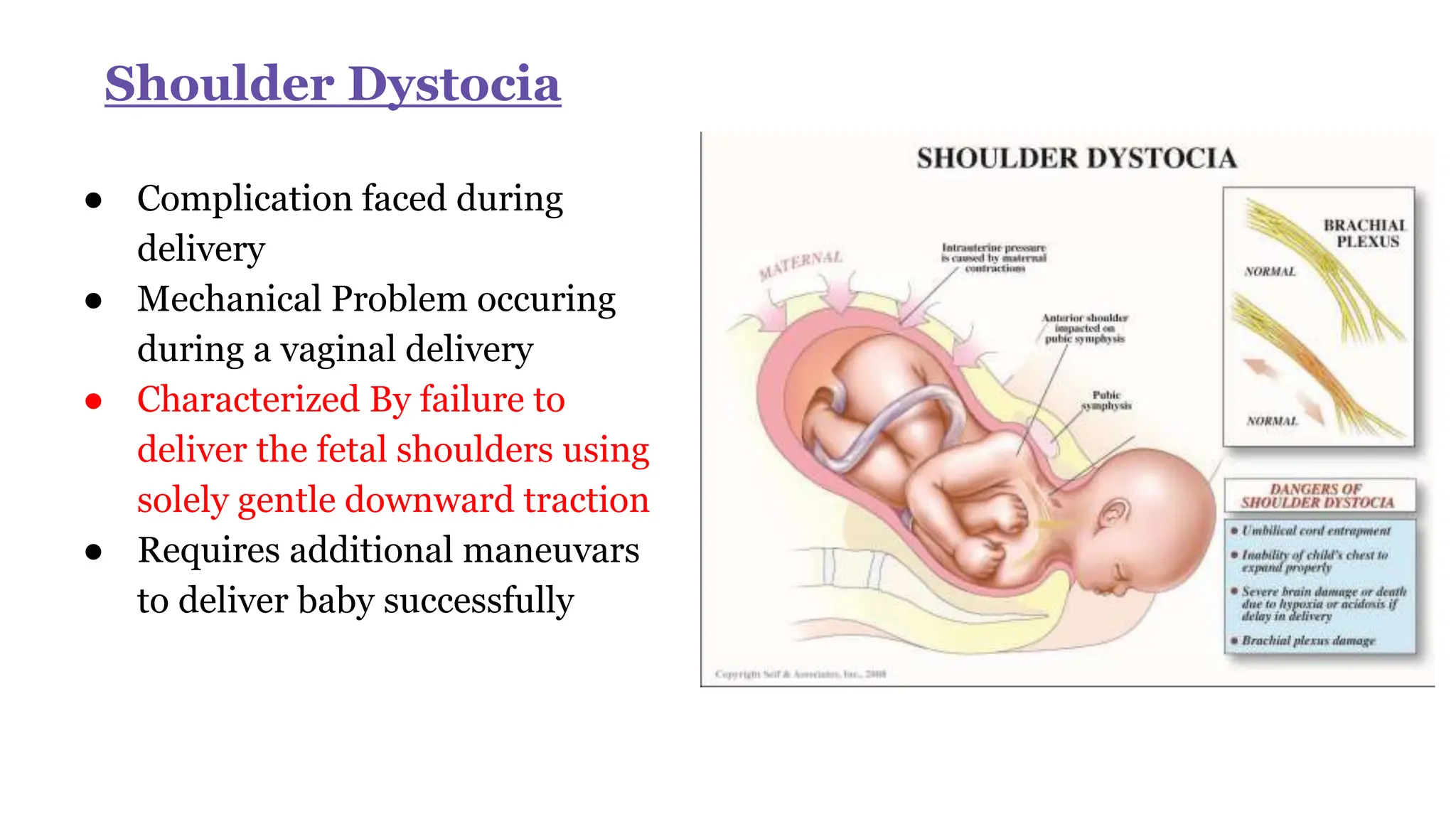
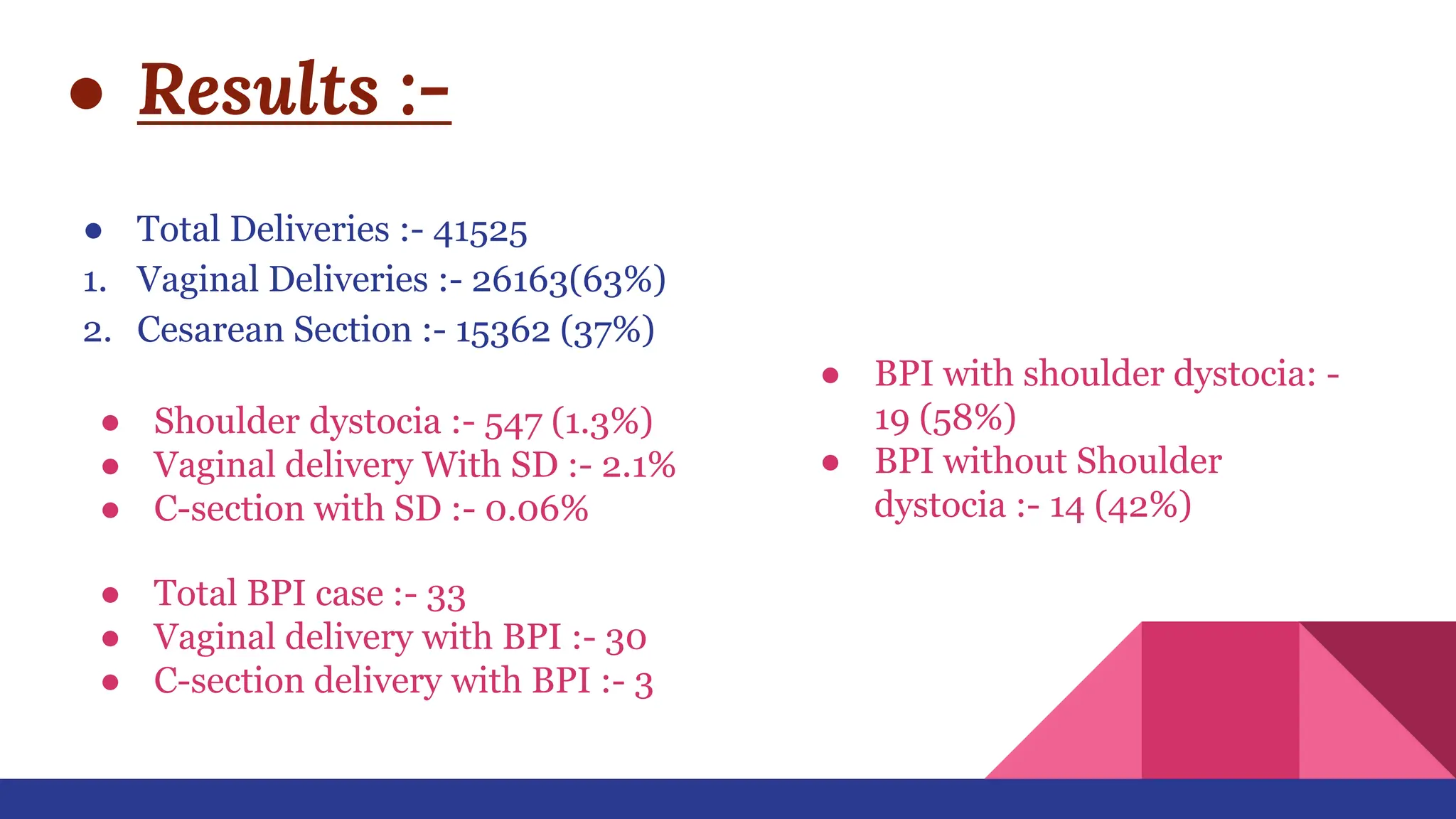
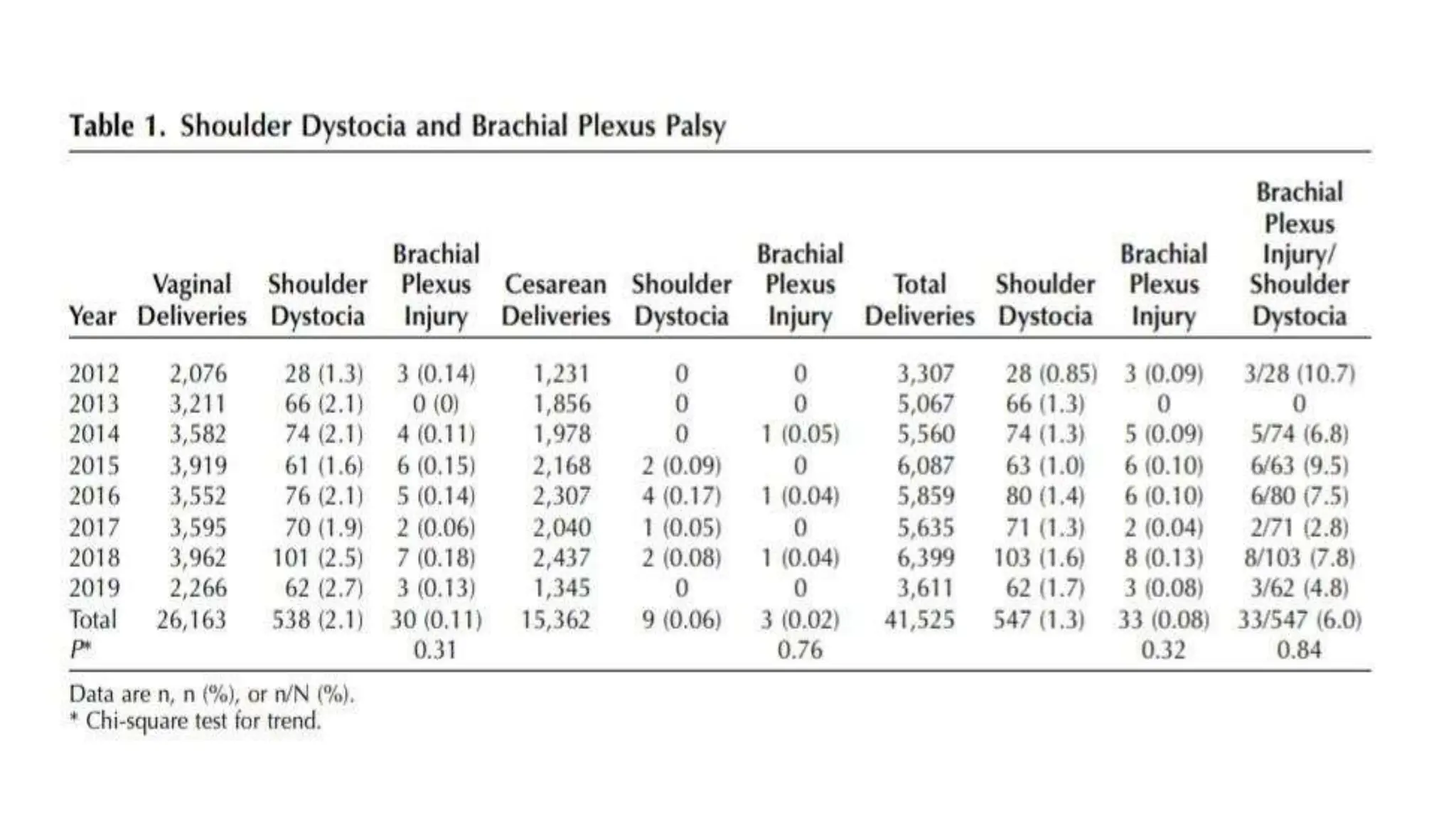
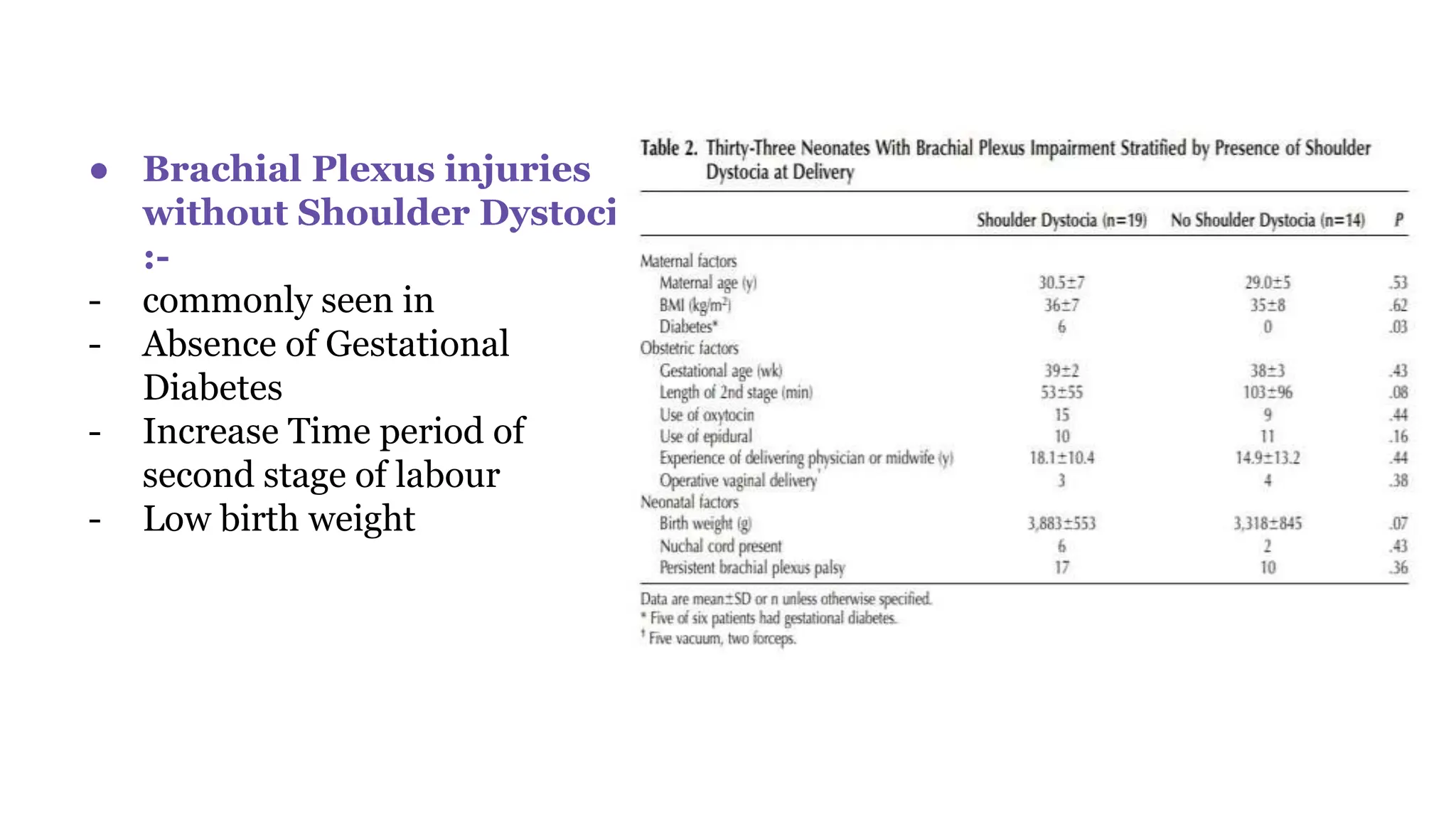
This study analyzed 33 cases of brachial plexus injury (BPI) that occurred during or after delivery at a single institution over time. The study found that 58% of BPI cases were associated with shoulder dystocia, while 42% occurred without shoulder dystocia. BPI without shoulder dystocia was associated with longer second stage of labor, low birth weight, and absence of gestational diabetes. The study concluded that both BPI and shoulder dystocia represent complications of uterine forces during delivery when there is disproportion between the fetal shoulders and birth canal, but they are not always causally related. Proper labor management and treatment of complications can help reduce the risk of BPI.