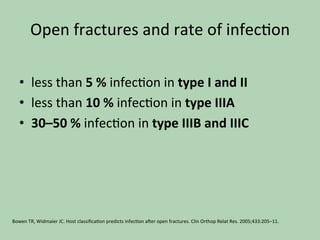
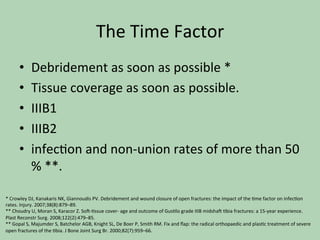
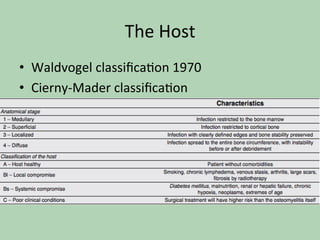
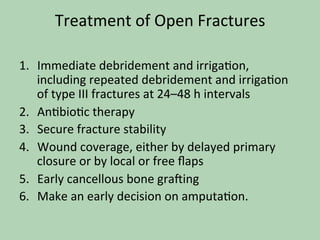
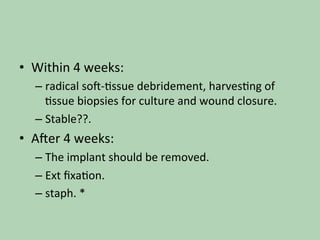
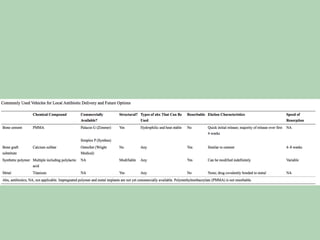
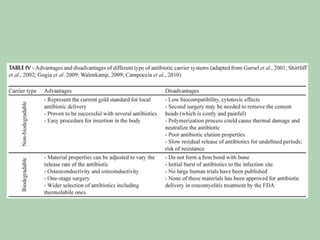
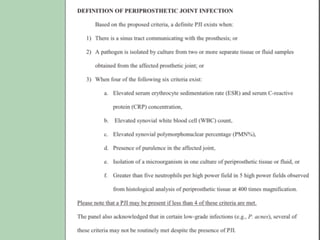
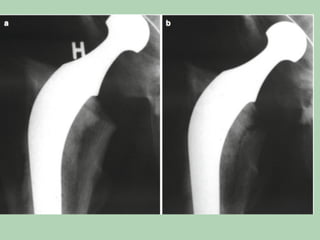
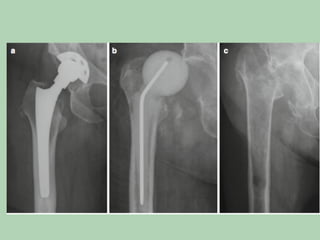
This document discusses post-traumatic and post-surgical bone infections. It covers infected fractures including open fractures classified using the Gustilo system, as well as post-operative infections in closed fractures treated with internal fixation. It also discusses prosthetic joint infections, how they are classified, diagnosed, and treated through options like debridement, revision surgery, or amputation. Throughout, it emphasizes the importance of early treatment and debridement to prevent infection.