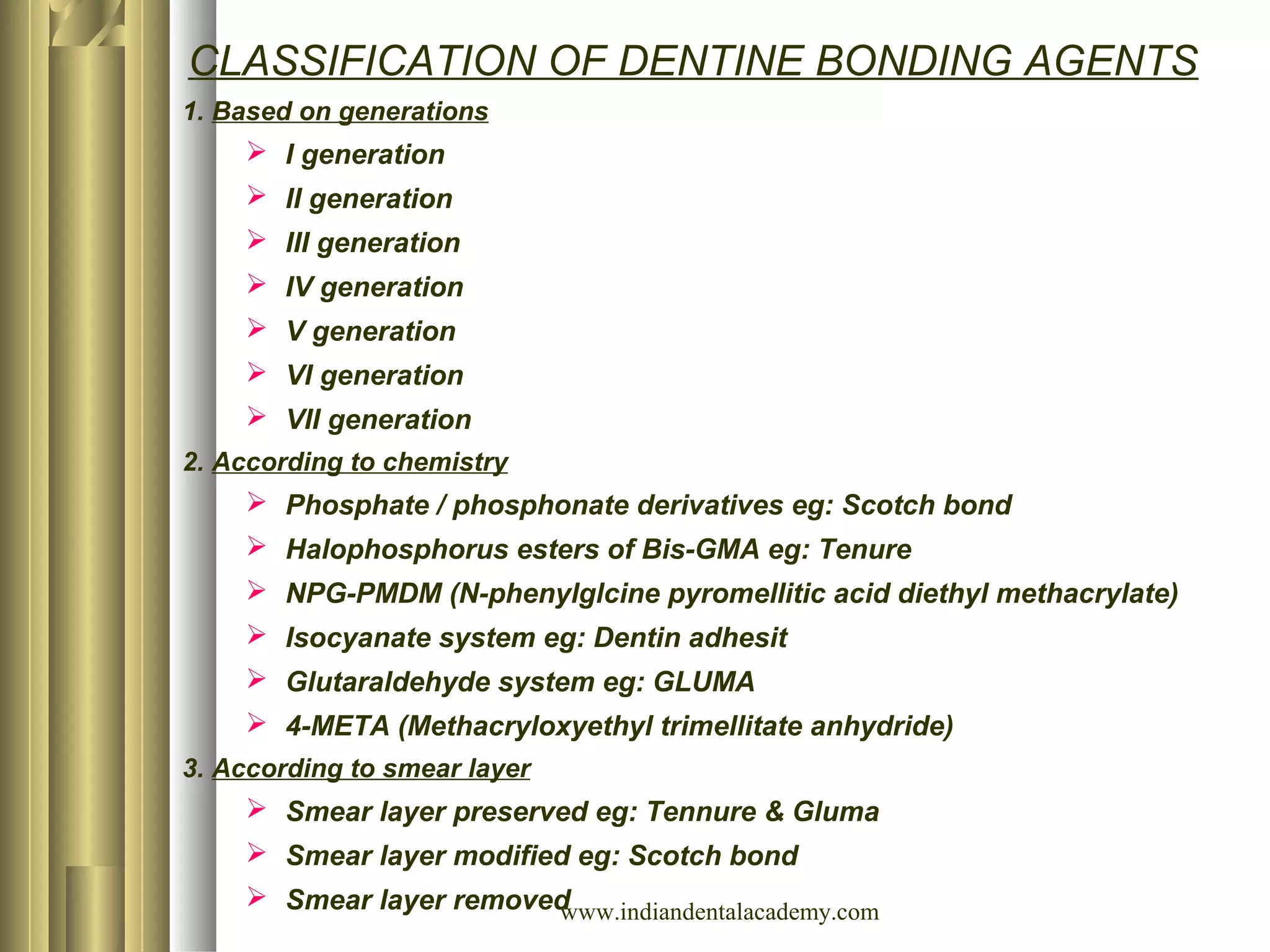
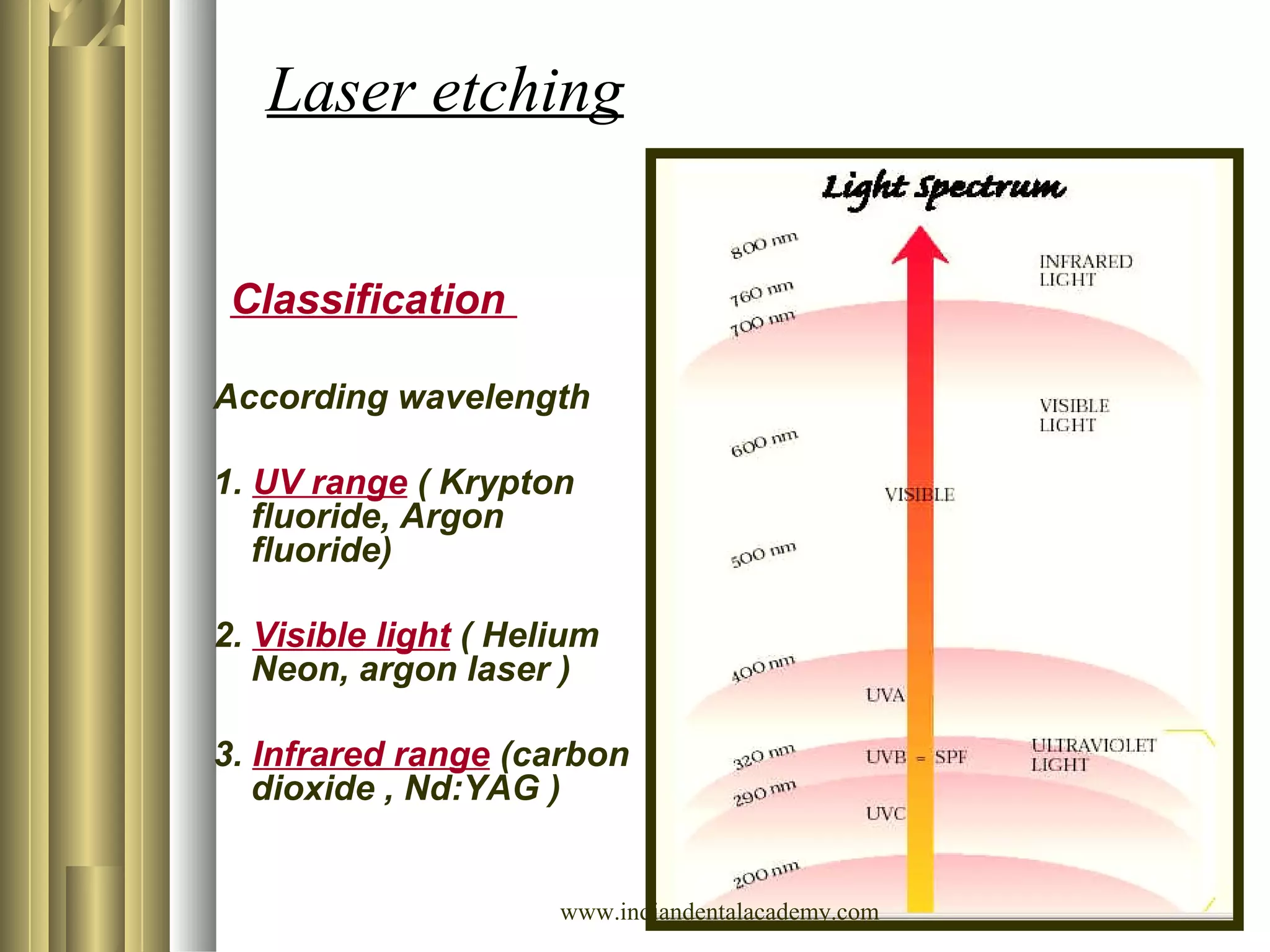
The document outlines the evolution and techniques of direct bonding in orthodontics, highlighting its significant development since the 1950s with contributions from various researchers. It discusses the advantages and disadvantages of direct bonding compared to traditional banding methods, as well as the types of bonding agents and their classifications. Additionally, it reviews historical milestones, adhesive systems, and the importance of creating ideal bonding conditions for orthodontic applications.