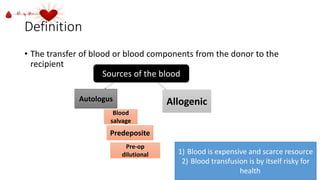
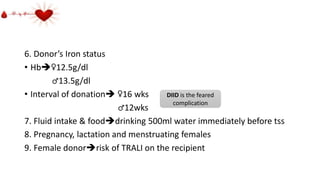
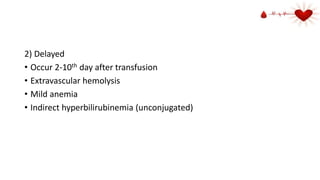
The document provides a comprehensive history and overview of blood transfusion practices, highlighting key milestones, figures of blood collection, and the evolution of blood banks in Ethiopia. It emphasizes the importance of donor health assessment, safety measures, and complications associated with blood transfusions. Furthermore, it discusses various blood components, their uses, and the potential risks and benefits of transfusion procedures.