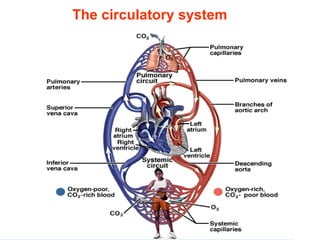
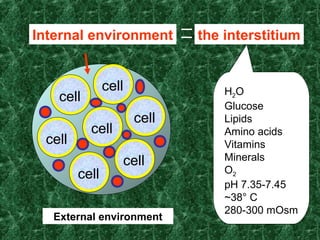
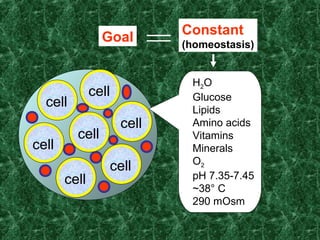
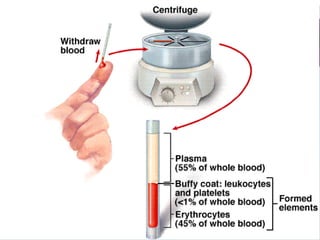
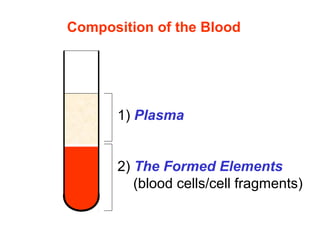
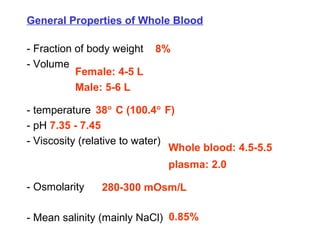
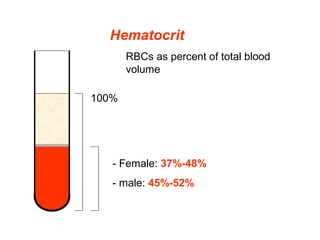
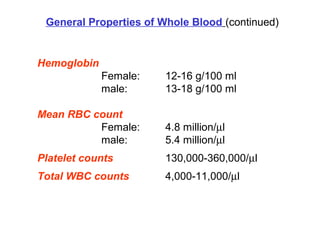
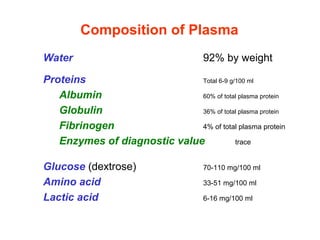
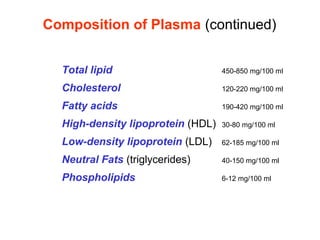
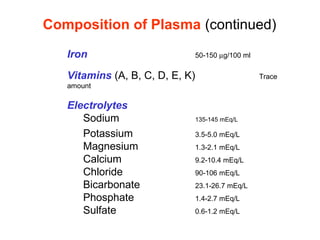
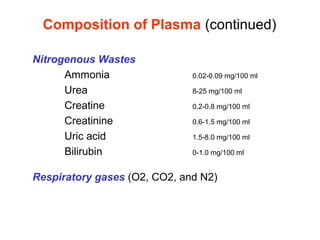
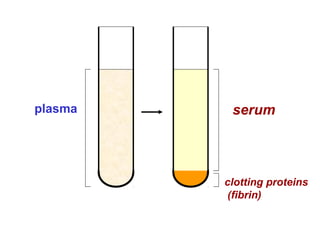
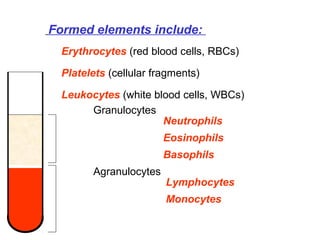
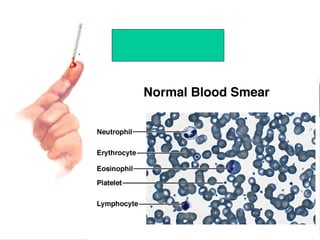
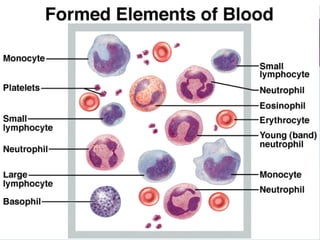
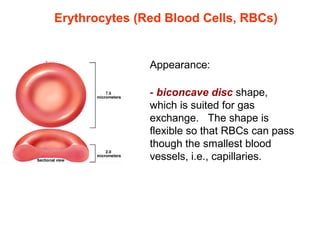
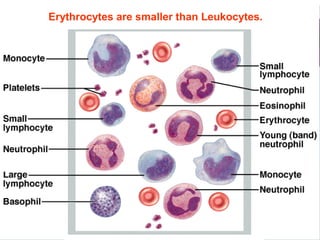
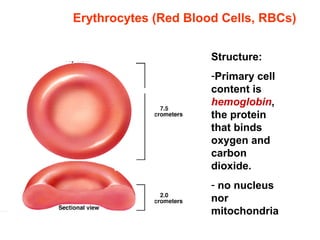
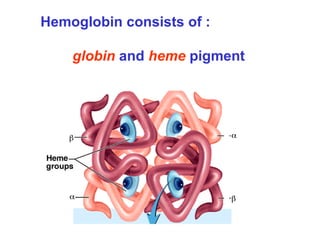
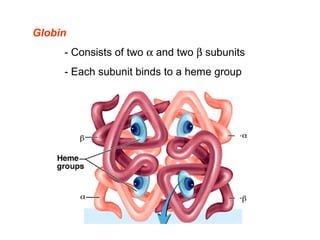
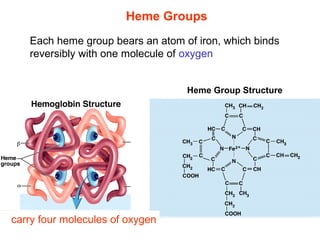
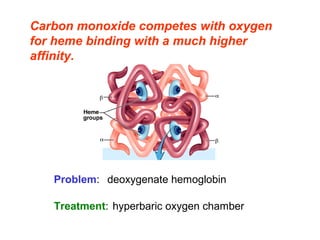
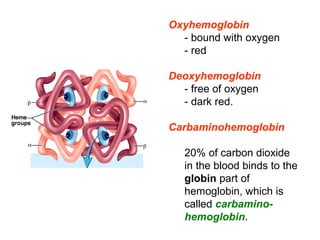
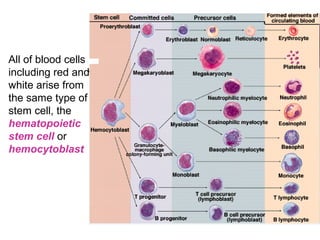
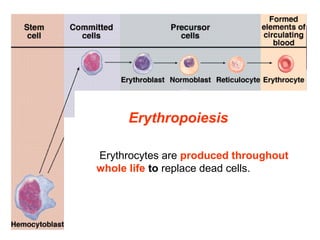
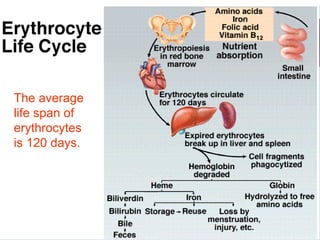
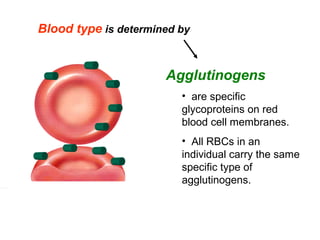
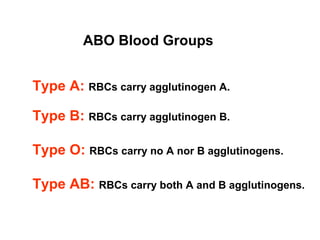
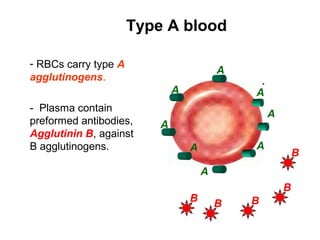
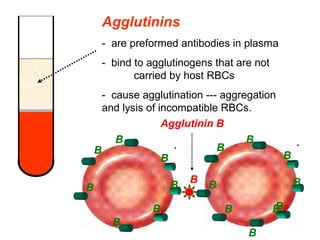
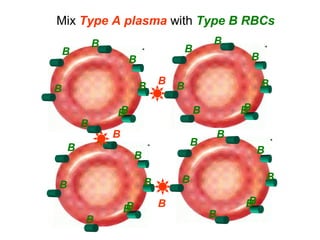
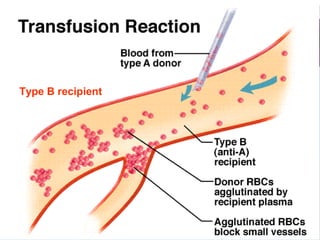
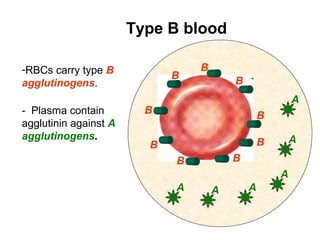
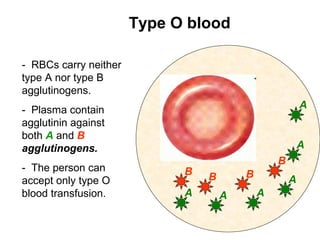
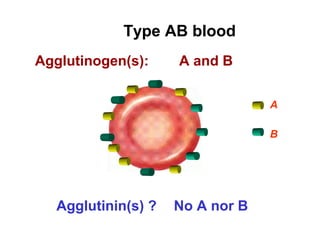
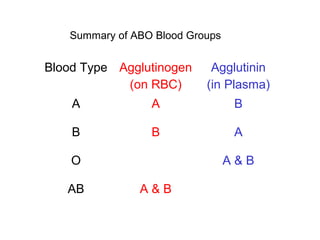
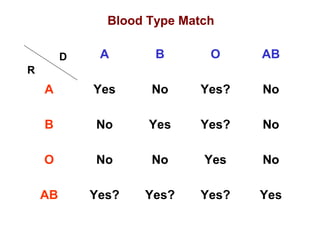
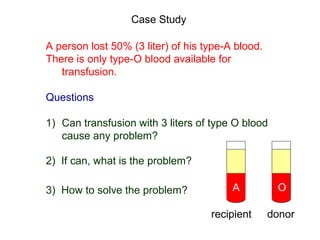
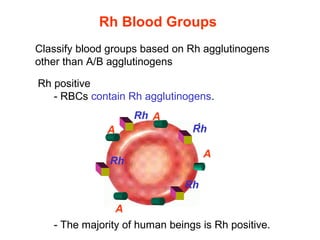
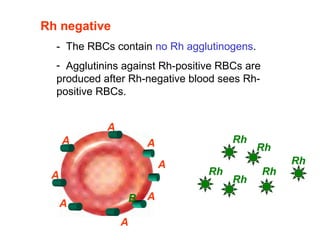
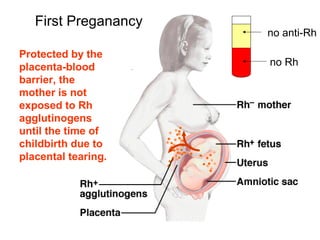
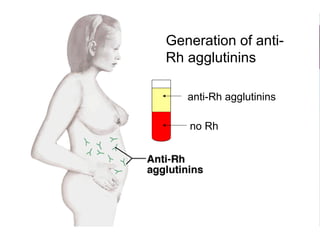
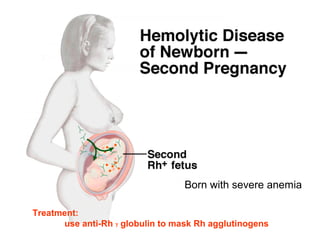
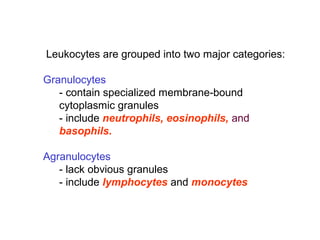
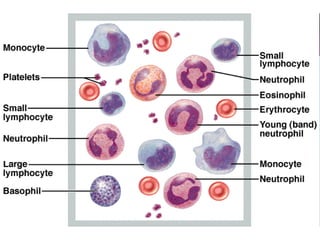
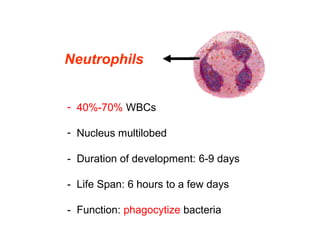
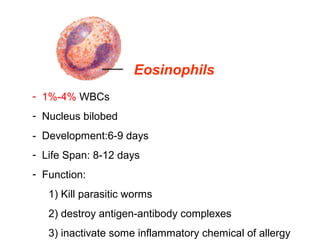
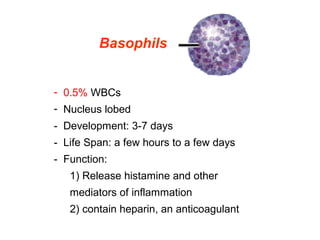
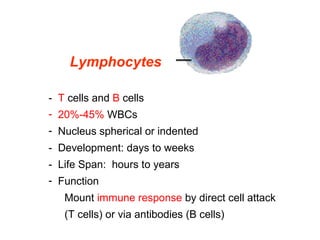
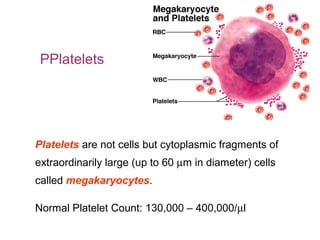
The circulatory system document discusses the circulatory system and blood. It provides an overview of blood components including plasma, which contains water, proteins, electrolytes and other substances, and formed elements such as erythrocytes, leukocytes and platelets. Erythrocytes contain hemoglobin which transports oxygen and carbon dioxide. Blood groups are determined by agglutinogens on red blood cells and agglutinins in plasma.