This document summarizes findings from a seminar on platelet and coagulation disorders. It includes:
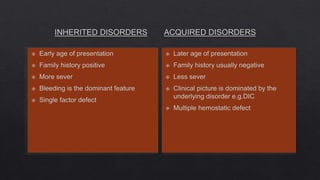
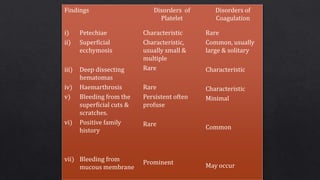
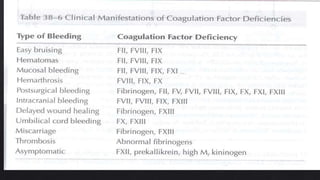
1. A table listing common clinical manifestations associated with specific hemostatic disorders, such as mucocutaneous bleeding seen in thrombocytopenias and platelet dysfunction disorders.
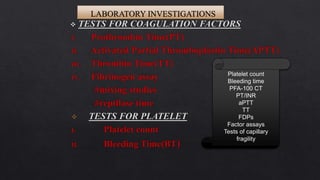
2. A list of laboratory tests useful in evaluating patients for platelet and coagulation disorders, including platelet count, bleeding time, and assays to measure coagulation factor levels.
3. A note that hemorrhagic stroke, surgical bleeding, and traumatic hemorrhage can occur in patients with underlying hemostatic disorders.