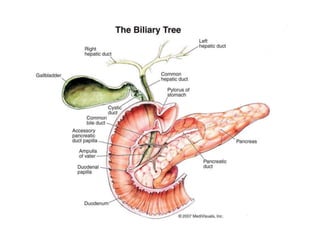
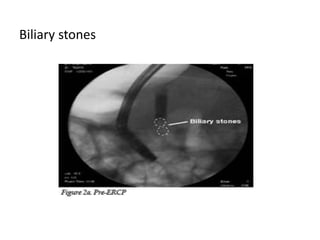
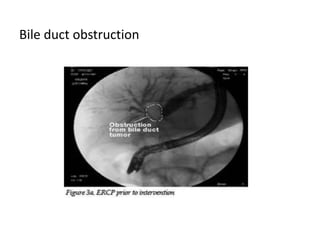
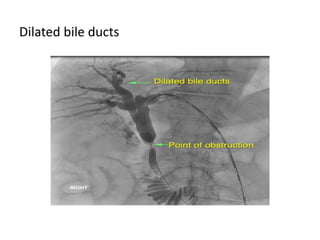
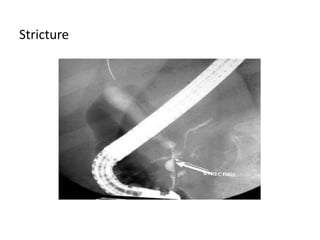
ERCP is an endoscopic procedure used to examine the duodenum, bile ducts, gallbladder, and pancreatic duct. A endoscope is inserted through the mouth and stomach to access the papilla of Vater. Contrast dye is injected through the endoscope to allow visualization of the bile and pancreatic ducts via x-ray imaging. Sedation is provided during the procedure. Potential risks include infection, pancreatitis, and perforation of the GI tract, though complications are less than 10% when performed by an experienced doctor.