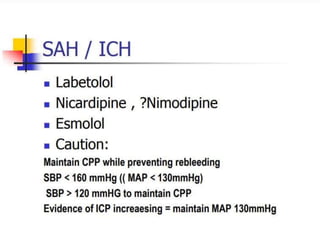
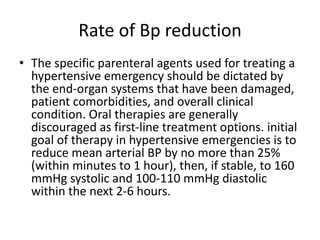
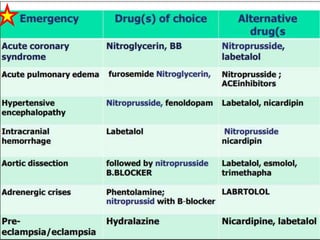
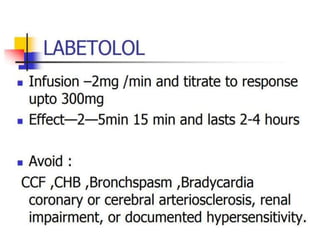
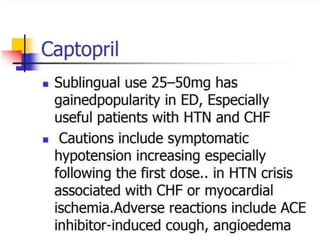
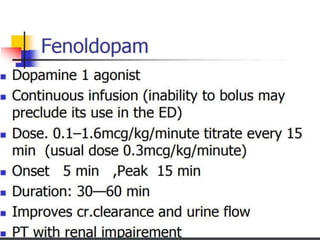
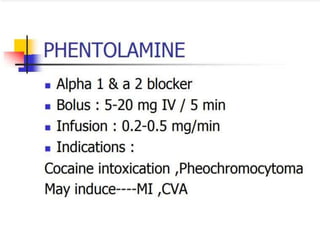
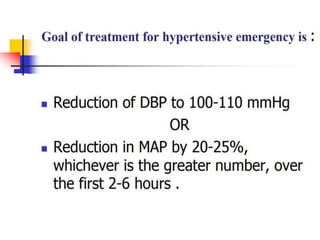
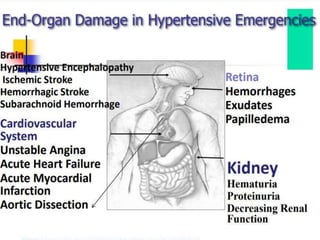
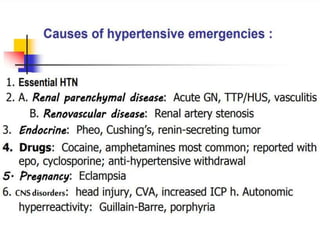
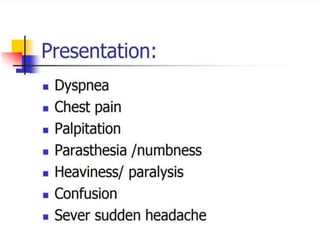
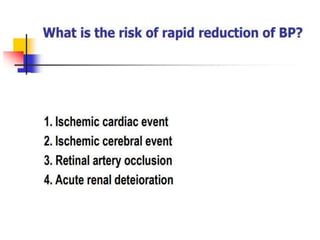
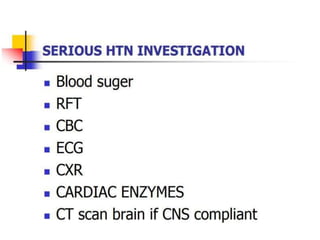
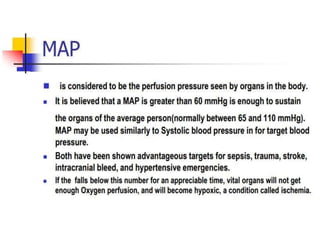
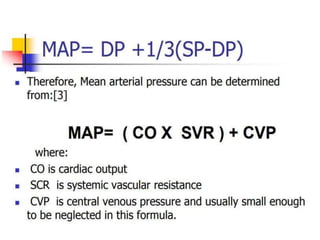
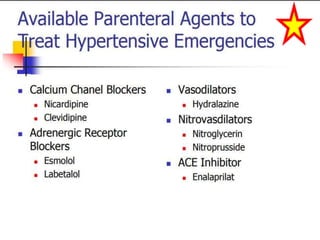
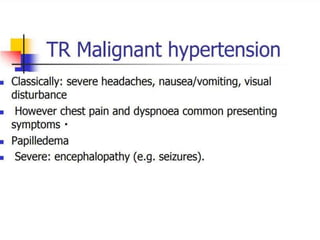
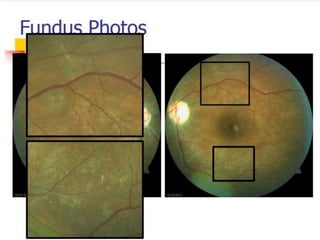
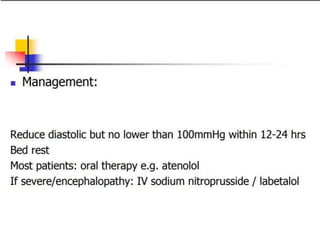
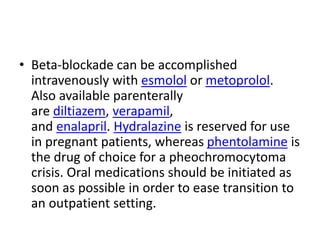
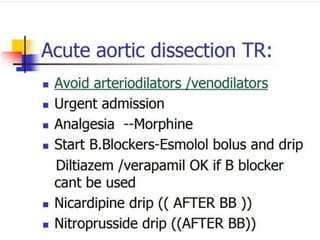
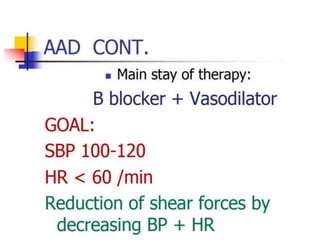
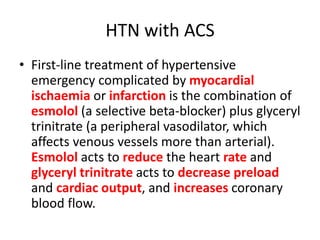
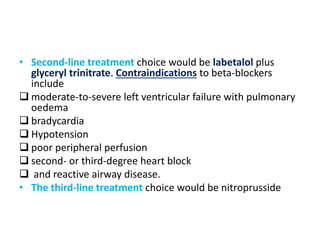
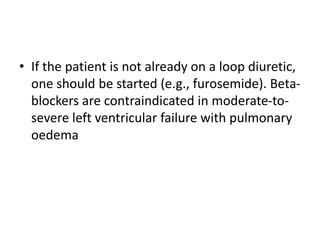
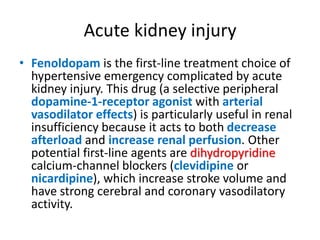
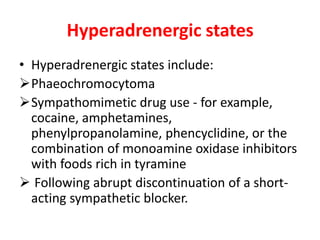
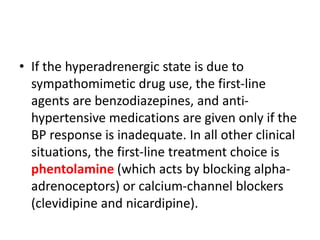
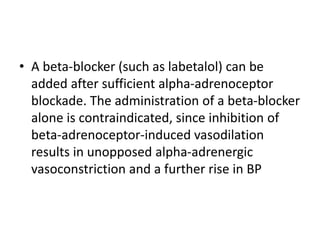
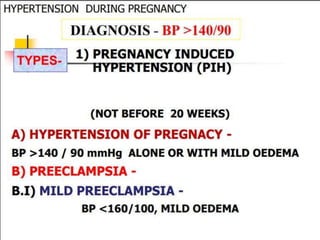
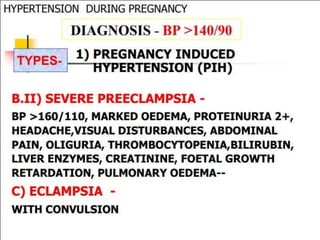
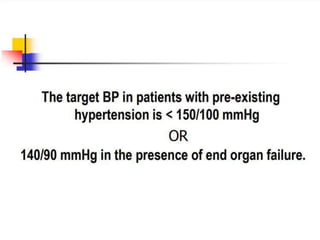
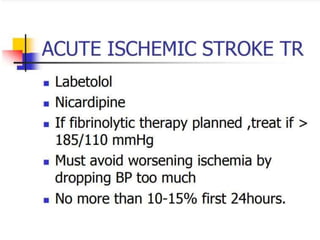
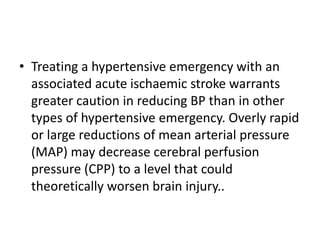
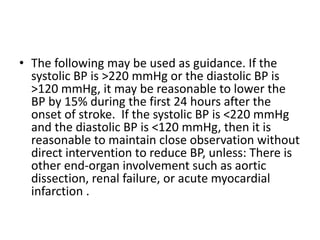
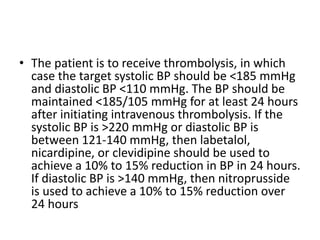
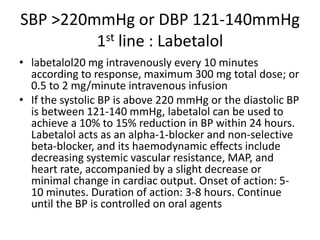
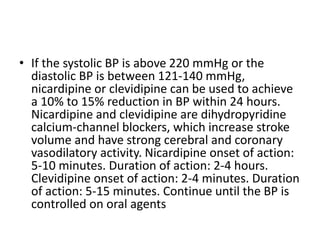
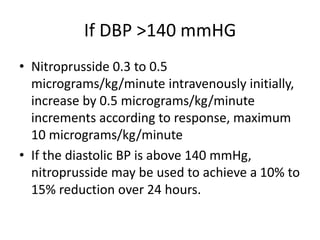
The document discusses guidelines for treating various hypertensive emergencies. It recommends first-line intravenous drugs like nitroprusside, fenoldopam, and labetalol. It provides guidance on treating specific complications like acute coronary syndrome, left ventricular failure, acute kidney injury, hyperadrenergic states, and acute ischemic stroke. The goal is to lower blood pressure no more than 25% initially and further gradually over 24-48 hours, avoiding excessive drops while stabilizing the patient. Exceptions are made for specific conditions like aortic dissection that require faster normalization.
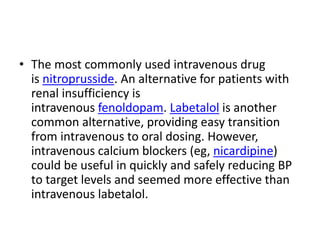
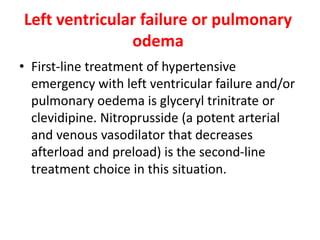
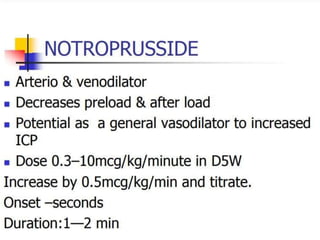
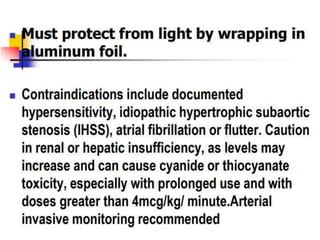
![• It acts as a potent arterial and venous vasodilator,
thereby reducing afterload and preload. Its
haemodynamic effects are to decrease MAP, with a
modest increase or no change in cardiac output. Onset
of action: immediate. Duration of action: 3-5 minutes.
Patients should be monitored by drawing thiocyanate
levels after 48 hours of therapy (levels maintained
<2064 micromol/L [<12 mg/dL or 120 mg/L]). The
maximum dose should be delivered for less than 10
minutes to decrease the chance of cyanide toxicity.
Continue until the BP is controlled on oral agents
•](https://image.slidesharecdn.com/htner-210906022614/85/hypertension-emergencies-46-320.jpg)