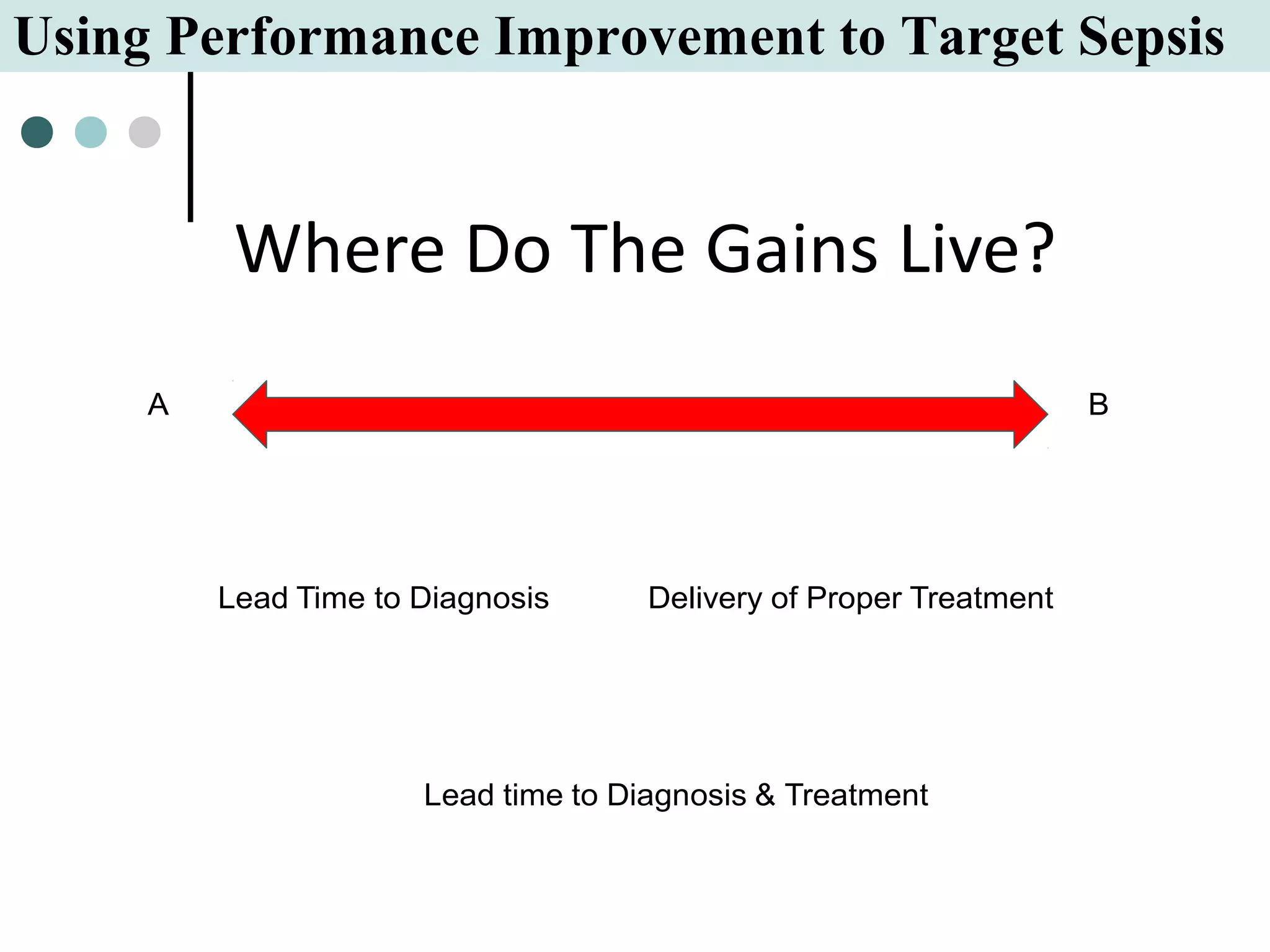
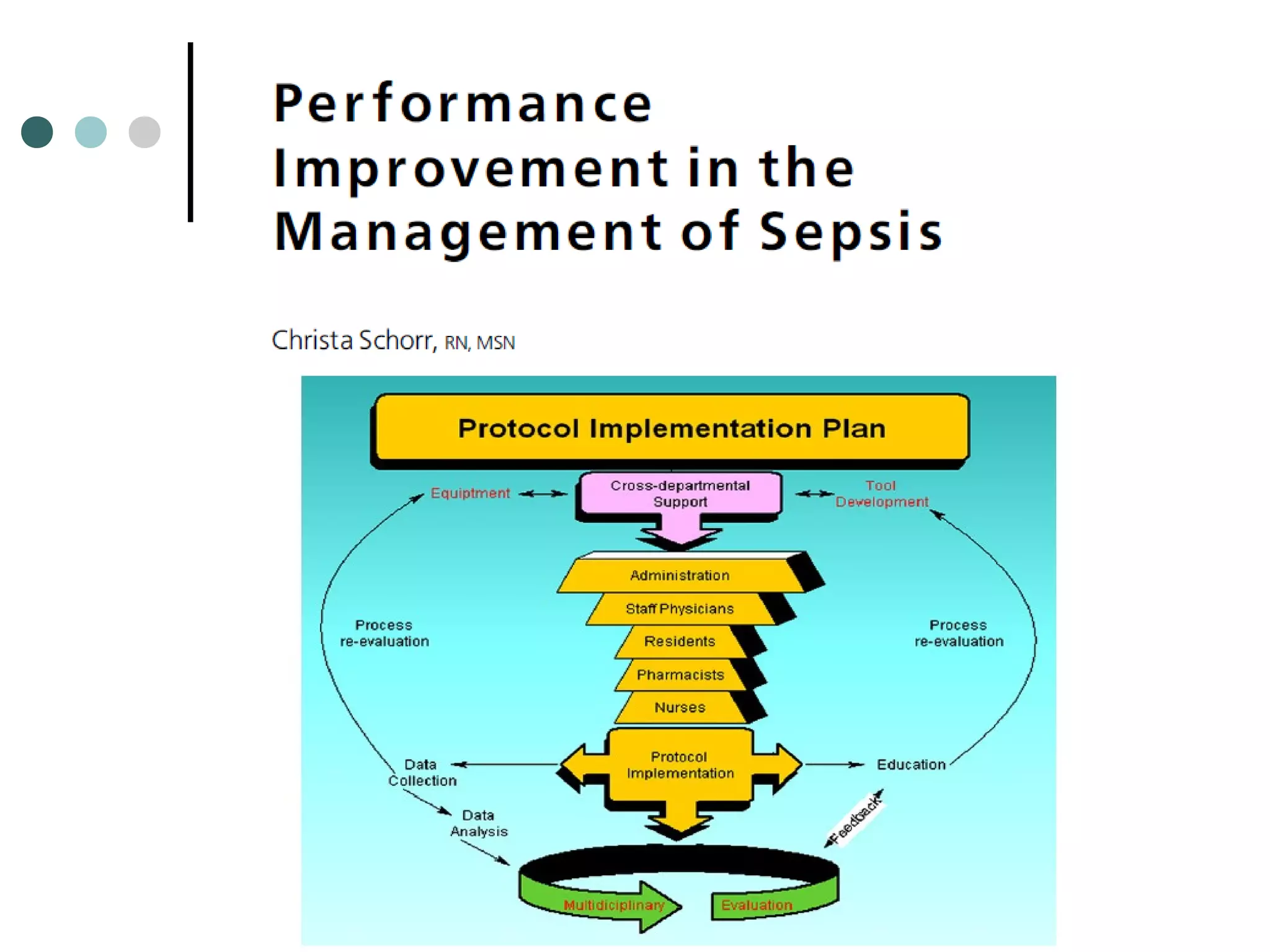
This document discusses the implementation of clinical practice guidelines for sepsis, specifically the Surviving Sepsis Campaign guidelines. It finds that while guidelines can be helpful, they are often not followed by more than 50% of clinicians. The document presents strategies to improve adherence through performance improvement initiatives at one medical center. These include identifying gaps in timely screening, diagnosis, initial resuscitation, antibiotics, and addressing goals of care. The focus is on both early identification and treatment of sepsis as well as the critical role of nurses in performance improvement efforts to optimize outcomes for patients with sepsis.

















![Basic care tasks [microbiological sampling and antibiotic delivery
within 1 hour, fluid resuscitation, and risk stratification using serum
lactate] are likely to benefit patients most, yet are unreliability performed.
Barriers include lack of awareness, lack of supporting controlled trials
and complex diagnostic criteria leading to recognition delays.](https://image.slidesharecdn.com/kleinpellsepsisifad2013finalrevised-161014095259/75/Applying-the-Surviving-Sepsis-Campaign-Guidelines-to-Clinical-Practice-18-2048.jpg)