The document is a November 2010 issue of the BC Medical Journal, focusing on surgical interventions for osteoarthritis of the hip and knee, including arthroscopy and joint replacement techniques. It also discusses various editorials, opinions on medical practices, and contributions from different authors on topics affecting healthcare. Additionally, it highlights the importance of using recycled paper for environmental benefits and features a farewell to a long-serving medical staff secretary in a community hospital.






![www.bcmj.org VOL. 52 NO. 9, NOVEMBER 2010 BC MEDICAL JOURNAL 435
Re: Medical
marijuana
W
hile Health Canada has
delegated responsibility to
physicians to recommend
the use of cannabis for access to their
legal program, it has clearly abdicated
its responsibility to educate doctors to
ensure their medical opinion is more
informed than that of DrVroom [Med-
ical marijuana. BCMJ 2010;52:329].
As a result, Dr Vroom is not alone
is his lack of knowledge about the
medical use of cannabis. During our
many years working and conducting
research at both the British Columbia
Compassion Club Society and the
Vancouver Island Compassion Soci-
ety, we have heard the other side of
doctor-patientdynamicthatDrVroom
describes.
Many patients report having an
extremely difficult time obtaining
support from their physicians for the
use of this medicine, or even dis-
cussing this legitimate health option.
This deeply affects the doctor-patient
relationship, causing patients unnec-
essary stress and creating an atmos-
phere of shame and distrust. Sadly,
many patients find themselves in the
role of having to educate their doctors.
Cannabis is a legal therapy option
officially sanctioned by the federal
government.Itisnotaphysician’srole
to decide what is or isn’t a medicine,
but rather to discuss the suitability of
treatment options on a case-by-case
basis.Inapreviouseditorial,DrVroom
stated,“Iamnotafraidtokeepanopen
mind about remedies I know nothing
about, but I research their scientific
evidence.”1 DrVroomseemstobemak-
ingan exception for medical cannabis.
Thousands of peer-reviewed sci-
entific studies have been published on
the use of cannabis to treat many dif-
ferent conditions and symptoms—as
personal view
Letters for Personal View are welcomed.
They should be double-spaced and less
than 300 words. The BCMJ reserves the
right to edit letters for clarity and length.
Letters may be e-mailed (journal@bcma
.bc.ca), faxed (604 638-2917), or sent
through the post.
MARKET LOSS RECOVERY GROUPMARKETT LOSS RECOV Y GROUPRVE
Continued on page 436](https://image.slidesharecdn.com/bcmj52vol9nov2010final-101123092531-phpapp02/85/British-Columbia-Medical-Journal-November-2010-7-320.jpg)

















![BC MEDICAL JOURNAL VOL. 52 NO. 9, NOVEMBER 2010 www.bcmj.org454
mentRegistry.Annualreport2008.www
.dmac.adelaide.edu.au/aoanjrr (acces-
sed 15 August 2009).
3. Walldius B. Arthroplasty of the knee joint
using an acrylic prosthesis. Acta Orthop
Scand 1953;23:121-131.
4. CharnleyJ.Arthroplastyofthehip.Anew
operation. Lancet 1961;1(7187):1129-
1132.
5. Gunston FH. Polycentric knee arthro-
plasty. Prosthetic simulation of normal
knee movement. J Bone Joint Surg Br
1971;53:272-277.
6. Ranawat CS. History of total knee
replacement. J South Orthop Assoc
2002;11:218-226.
7. Coventry MB, Finerman GA, Riley LH, et
al. A new geometric knee for total knee
arthroplasty. Clin Orthop Relat Res 1972;
83:157-162.
8. Freeman MA, Swanson SA, Todd RC.
Total replacement of the knee using the
Freeman-Swanson knee prosthesis. Clin
Orthop Relat Res 1973;(94):153-170.
9. Insall JF, Ranawat CS, Scott WN, et al.
Total condylar knee replacment: Prelimi-
nary report. Clin Orthop Relat Res
1976;149-154.
10. Ranawat CS, Shine JJ. Duo-condylar
total knee arthroplasty. Clin Orthop Relat
Res 1973;(94):185-195.
11. Townley C, Hill L. Total knee replace-
ment. Am J Nurs 1974;74:1612-1617.
12. McKeever DC. The classic: Tibial plateau
prosthesis 1960. Clin Orthop Relat Res
2005;440:4-8.
13. Goodfellow J, O’Connor J. The mechan-
ics of the knee and prosthesis design. J
Bone Joint Surg Br 1978;60-B:358-369.
14.Marmor L. The modular knee. Clin
Orthop Relat Res 1973;(94)242-248.
15. Smith DF, McGraw RW, Taylor DC, et al.
Arterial complications and total knee
arthroplasty. J Am Acad Orthop Surg
2001;9:253-257.
16. Lonner JH, Lotke PA. Aseptic complica-
tions after total knee arthroplasty. J Am
Acad Orthop Surg 1999;7:311-324.
17. Lie SA, Engesaeter LB, Havelin LI, et al.
Early postoperative mortality after
67,548 total hip replacements: Causes of
death and thromboprophylaxis in 68 hos-
pitals in Norway from 1987 to 1999. Acta
Orthop Scand 2002;73:392-399.
18. National Joint Registry [for England and
Wales 2007]. www.njrcentre.org.uk (ac-
cessed 13 September 2010).
19. Fang DM, Ritter MA, Davis KE. Coronal
alignment in total knee arthroplasty: Just
how important is it? J Arthroplasty 2009;
24:39-43.
20. Spalding TJ, Kiss J, Kyberd P, et al. Driv-
er reaction times after total knee replace-
ment. J Bone Joint Surg Br 1994;76:754-
756.
21. RanawatCS,RanawatAS,MehtaA.Total
knee arthroplasty rehabilitation protocol:
What makes the difference? J Arthro-
plasty 2003;18:27-30.
22. PradhanNR,GambhirAF,PorterML.Sur-
vivorship analysis of 3234 primary knee
arthroplasties implanted over a 26-year
period: A study of eight different implant
designs. Knee 2006;13:7-11.
23. Ranawat CS, Flynn WF Jr, Saddler S, et
al. Long-term results of the total condy-
lar knee arthroplasty. A 15-year survivor-
ship study. Clin Orthop Relat Res 1993;
(286)94-102.
24. Rodriguez JA, Bhende HF, Ranawat CS.
Total condylar knee replacement: A 20-
year followup study. Clin Orthop Relat
Res 2001;(388)10-17.
25. Pavone VM, Boettner FM, Fickert SM, et
al. Total condylar knee arthroplasty: A
long-term followup. Clin Orthop Relat
Res 2001;(388):18-25.
26. Ritter MA, Berend ME, Meding JB, et al.
Long-term followup of anatomic gradu-
ated components posterior cruciate-
retaining total knee replacement. Clin
Orthop Relat Res 2001;(388):51-57.
27. Ritter MA. The Anatomical Graduated
Component total knee replacement: A
long-term evaluation with 20-year sur-
vival analysis. J Bone Joint Surg Br
2009;91:745-749.
28. Berger RA, Rosenberg AG, Barden RM,
et al. Long-term followup of the Miller-
Galante total knee replacement. Clin
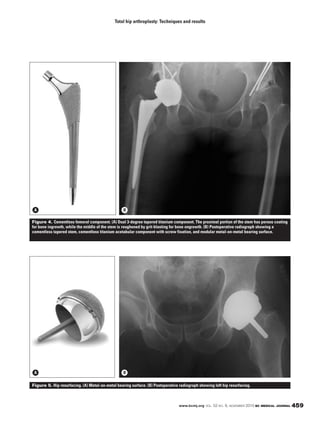
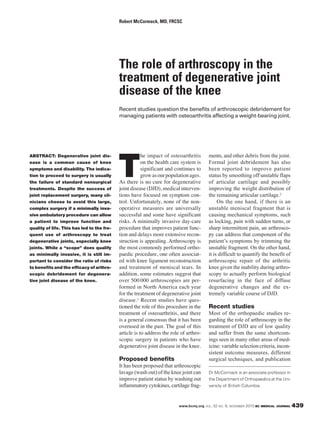
Total knee arthroplasty: Techniques and results
Orthop Relat Res 2001;(388):58-67.
29. Laskin RS. The Genesis total knee pros-
thesis: A 10-year followup study. Clin
Orthop Relat Res 2001;(388):95-102.
30. Berger RA, Meneghini RM, Jacobs JJ, et
al. Results of unicompartmental knee
arthroplasty at a minimum of ten years of
follow-up. J Bone Joint Surg Am
2005;87:999-1006.
31. Murray DW, Goodfellow JW, O’Connor
JJ. The Oxford medial unicompartmen-
tal arthroplasty: A ten-year survival study.
J Bone Joint Surg Br 1998;80:983-989.
32. Baker PN, van der Meulen JH, Lewsey
JF, et al. The role of pain and function in
determining patient satisfaction after
total knee replacement. Data from the
National Joint Registry for England and
Wales. J Bone Joint Surg Br 2007;
89:893-900.
33. Ranawat CS, Padgett DF, Ohashi Y. Total
knee arthroplasty for patients younger
than 55 years. Clin Orthop Relat Res
1989;(248)27-33.
34. Diduch DR, Insall JN, Scott WN, et al.
Total knee replacement in young, active
patients. Long-term follow-up and func-
tional outcome. J Bone Joint Surg Am
1997;79:575-582.
35. Griffin FM, Scuderi GR, Insall JN, et al.
Total knee arthroplasty in patients who
were obese with 10 years followup. Clin
Orthop Relat Res 1998;(356)28-33.
36. Gatha NM, Clarke HD, Fuchs RF, et al.
Factors affecting postoperative range of
motion after total knee arthroplasty. J
Knee Surg 2004;17:196-202.](https://image.slidesharecdn.com/bcmj52vol9nov2010final-101123092531-phpapp02/85/British-Columbia-Medical-Journal-November-2010-26-320.jpg)