This document discusses Barrett's esophagus, including its definition, diagnosis, clinical presentation, natural history, epidemiology, pathogenesis, and management. Key points include:
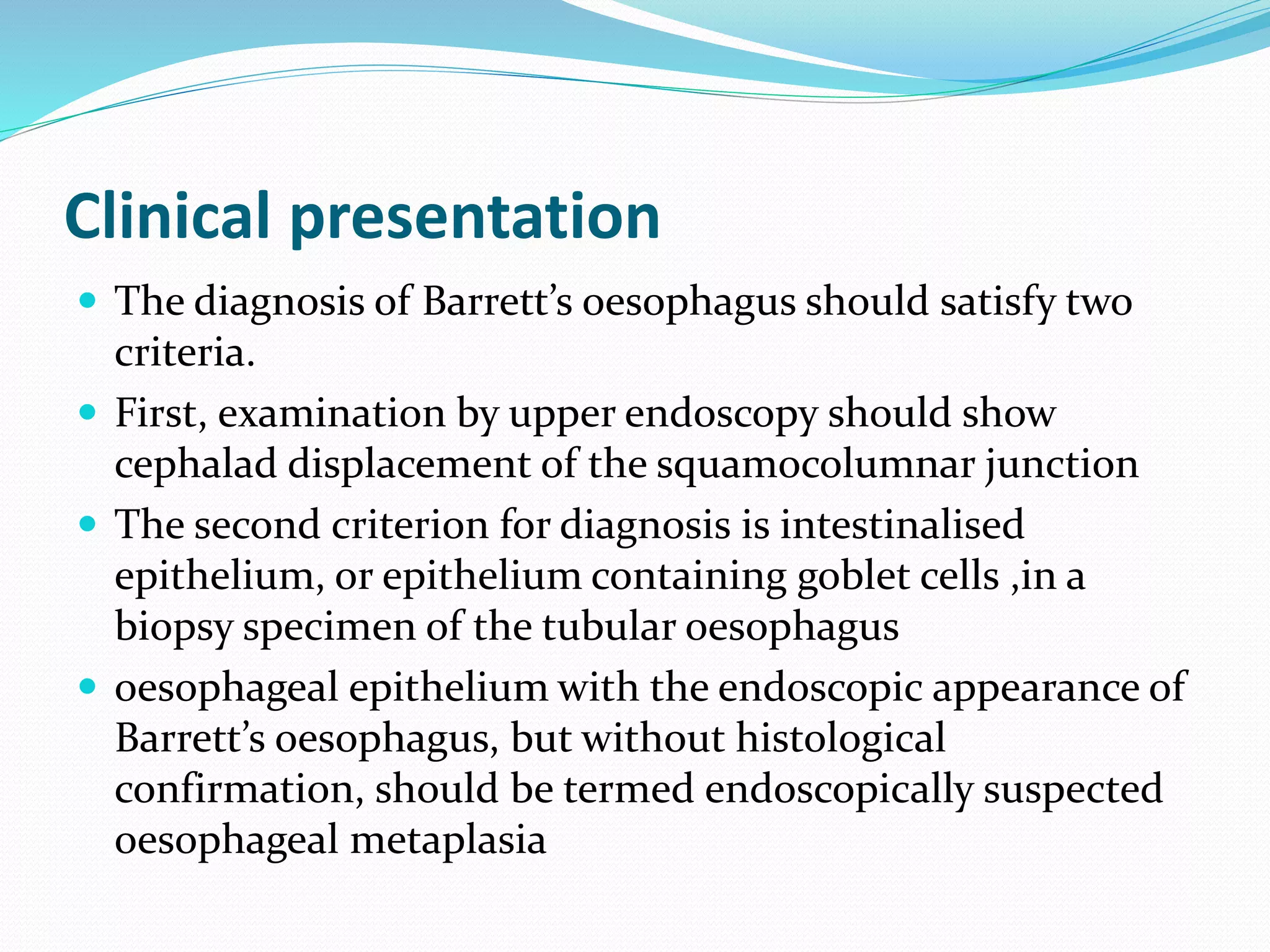
- Barrett's esophagus is diagnosed when endoscopy shows columnar-lined esophagus and biopsies confirm intestinal metaplasia. It is associated with increased risk of esophageal adenocarcinoma.
- Risk factors include chronic gastroesophageal reflux, white male sex, obesity, and central adiposity.
- Surveillance endoscopy is recommended for diagnosed Barrett's esophagus to screen for dysplasia or cancer. Histological confirmation of intestinal metaplasia is needed prior to initiating surveillance.