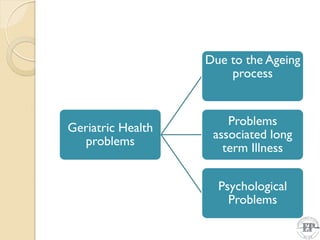
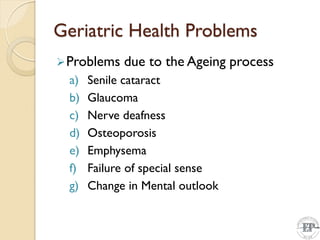
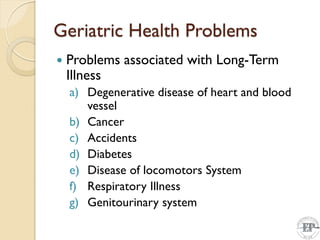
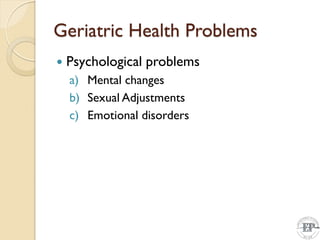
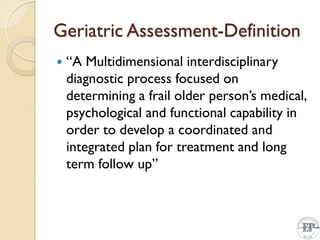
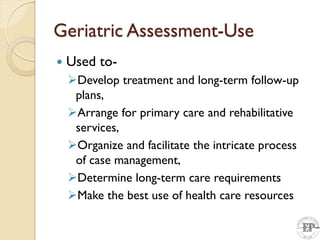
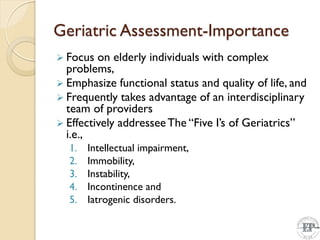
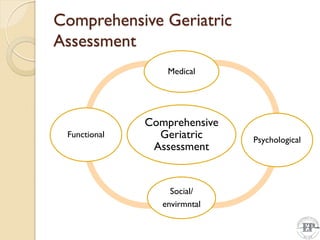
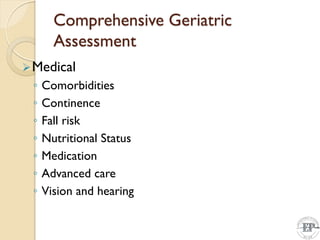
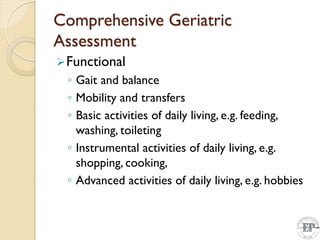
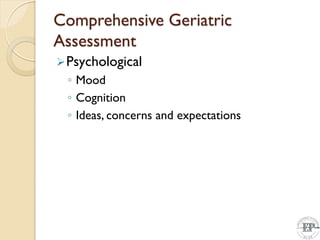
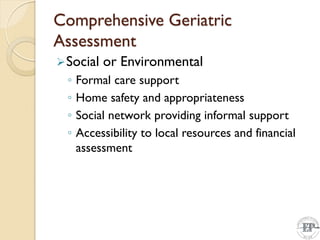
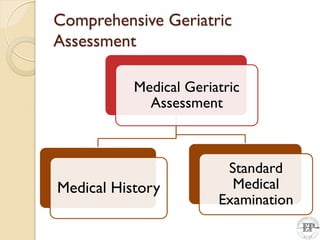
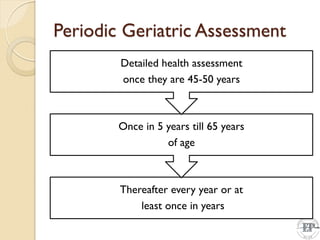
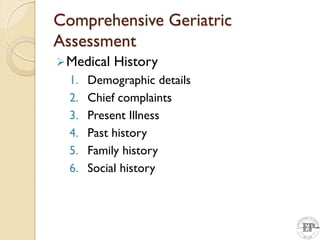
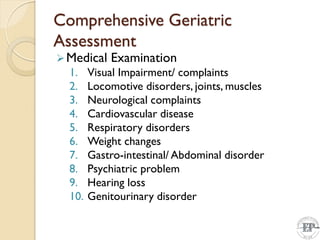
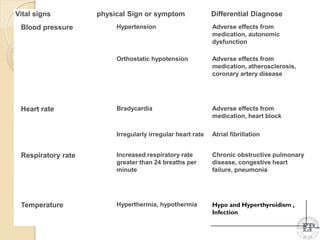
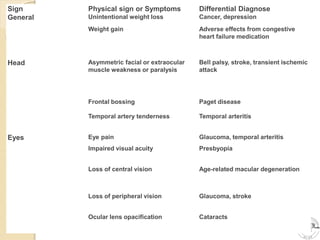
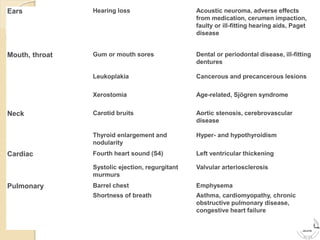
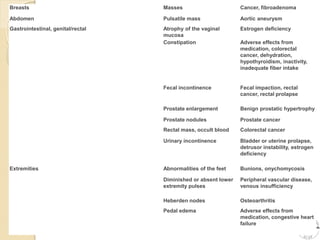
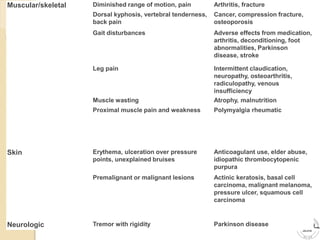
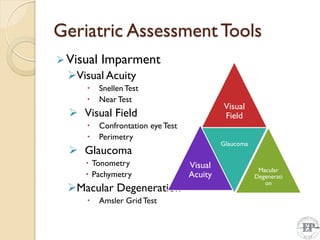
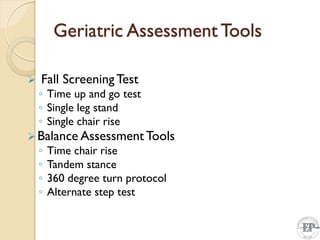
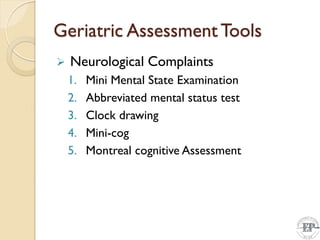
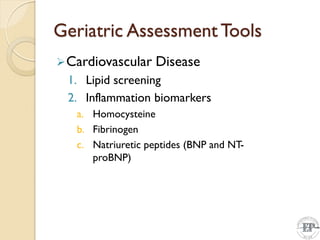
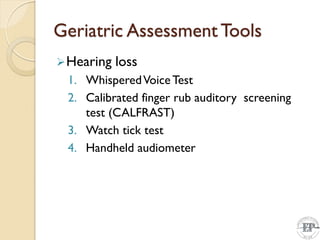
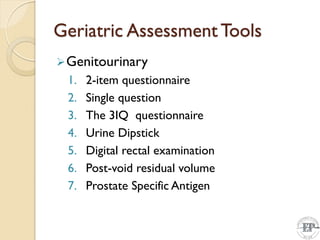
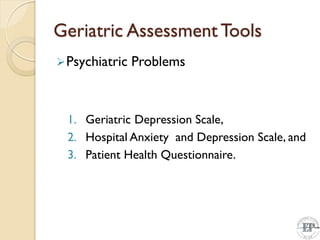
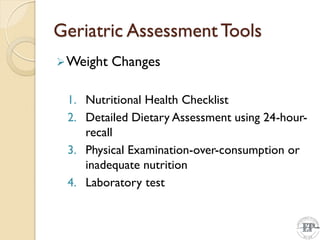
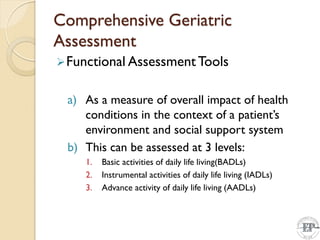
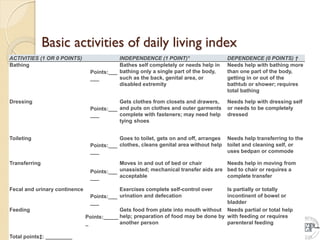
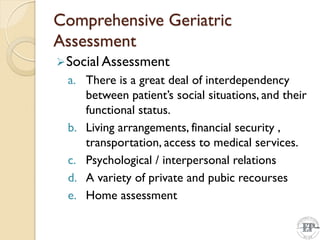
The document discusses the assessment of elderly clients, focusing on geriatrics and gerontology, which deal with health issues related to aging. It outlines the various health problems faced by older adults, the importance of comprehensive geriatric assessment in addressing medical, psychological, and functional capabilities, and the necessity for interdisciplinary care approaches. Additionally, it highlights key assessment tools and challenges associated with geriatric assessments.