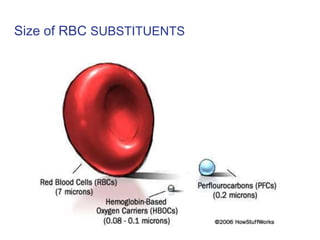
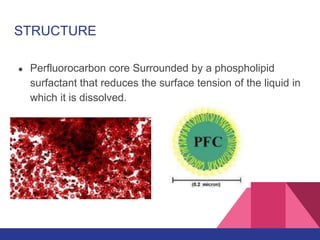
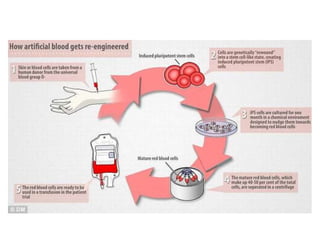
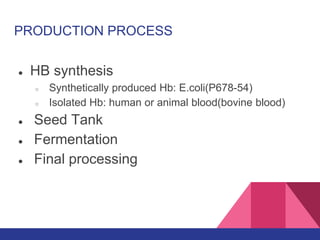
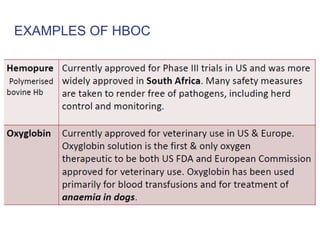
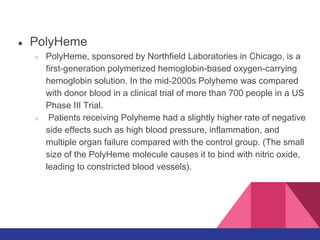
Artificial blood, also called blood substitutes, aims to provide an alternative to blood transfusions by mimicking some functions of biological blood without containing blood cells. The main advantages are longer shelf life, availability without matching blood types, and lower risk of disease transmission. Two main types are perfluorocarbons, which can dissolve oxygen but have low carrying capacity, and hemoglobin-based oxygen carriers produced from purified hemoglobin but which have shorter lifespans in the body. Both have shown promise in clinical trials but also safety issues like inflammation. Research continues to develop safer and more effective artificial blood.