This document provides a comprehensive overview of anemia, including its definition, classification, types, and diagnostic criteria. It highlights the prevalence of anemia in different populations, particularly in India, and discusses various causes, clinical presentations, and diagnostic investigations for different forms of anemia. Key takeaways include the importance of diagnosing underlying causes and recognizing iron deficiency as the most common type of anemia.

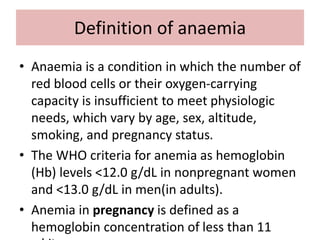




























![Diagnosis of hemolytic anemia
• General examination- Jaundice, pallor
• Other physical findings Splenomegaly; bossing of skull
• Hemoglobin level From normal to severely reduced
• MCV, MCH Usually increased
• Reticulocytes Increased
• Bilirubin Increased (mostly unconjugated)
• LDH Increased
• Haptoglobin Reduced to absent
• direct Coombs test [DAT] is an indicator of the presence of
antibodies attached to RBC.
• The indirect Coombs test indicates the presence of free
antibody in the plasma.
• A peripheral blood smear-in Intravascular hemolysis may
show red cell fragmentation (i.e., schistocytes,helmet cells)](https://image.slidesharecdn.com/aneamiadiagnosisbpharm-240730183232-bafb7193/85/Aneamia-diagnosis-and-classifications-Bpharm-pptx-31-320.jpg)









