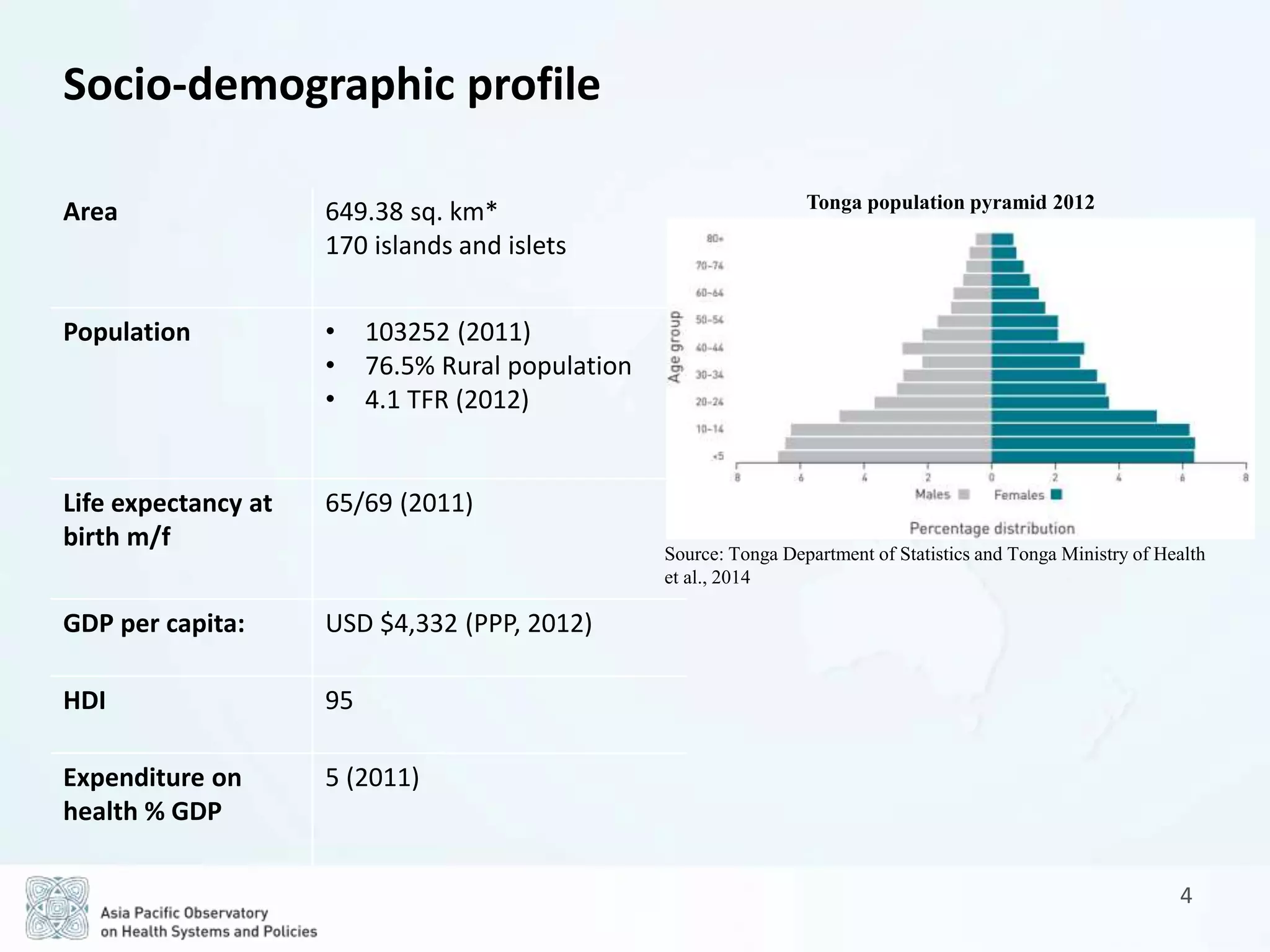
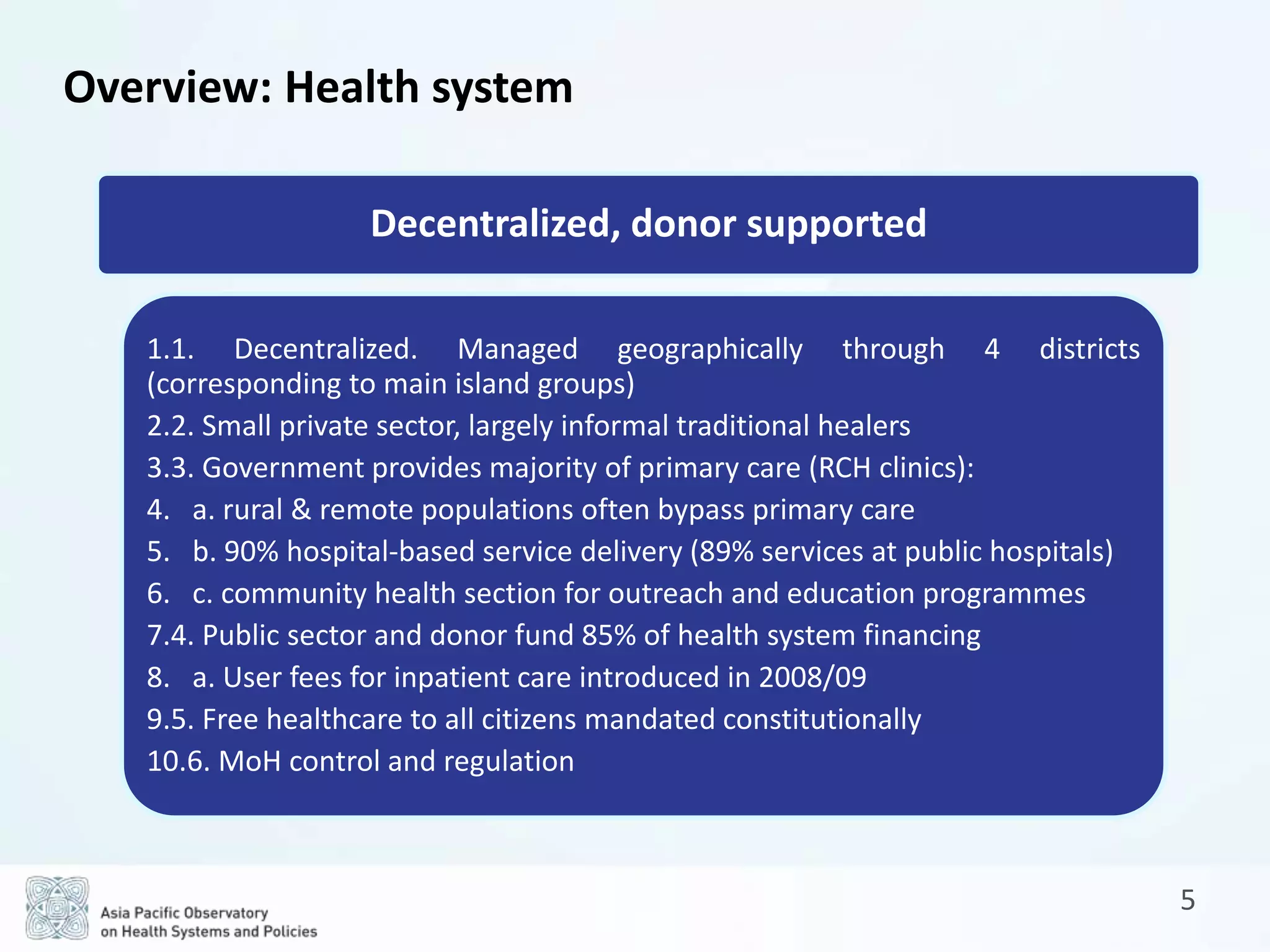
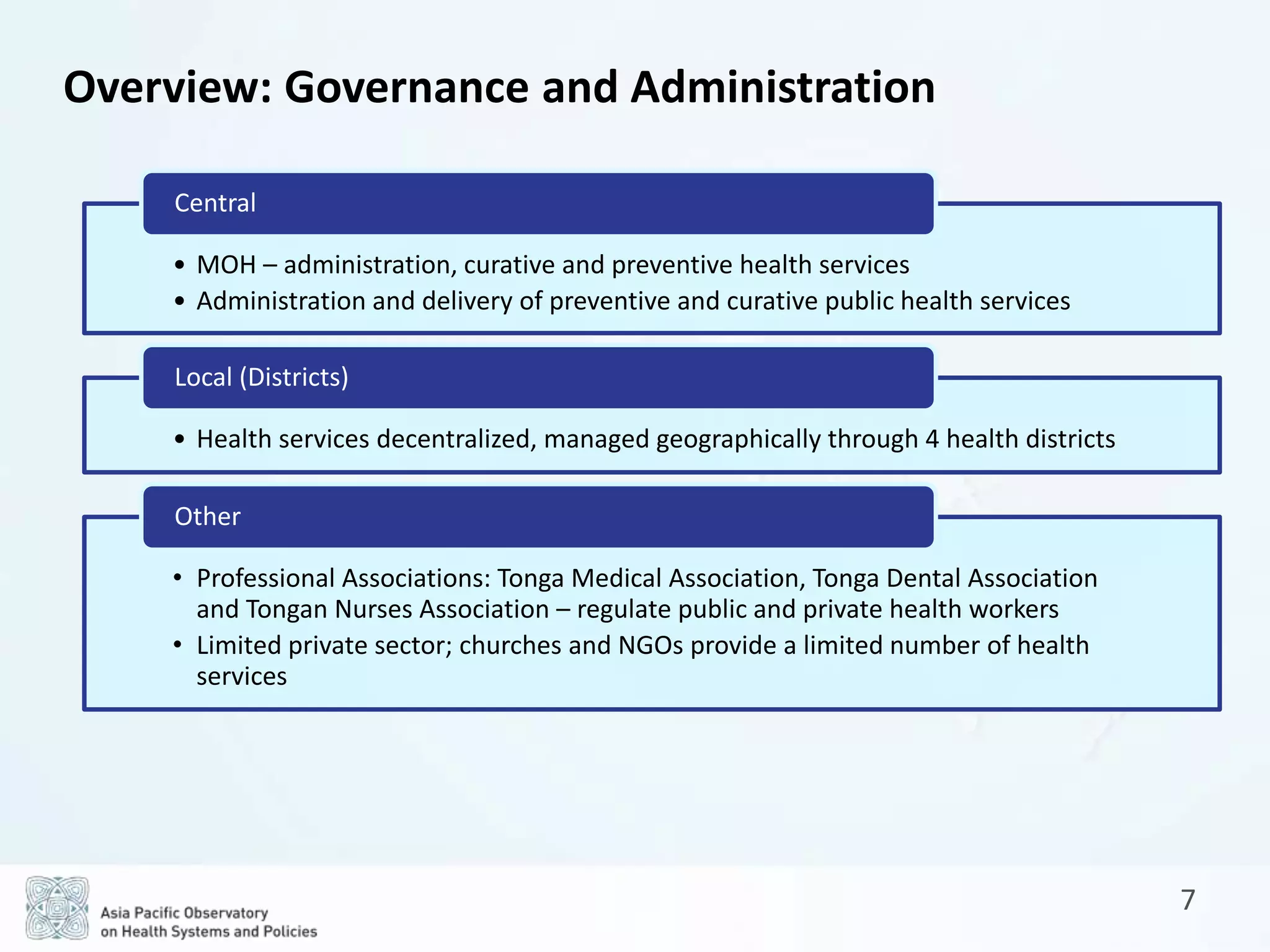
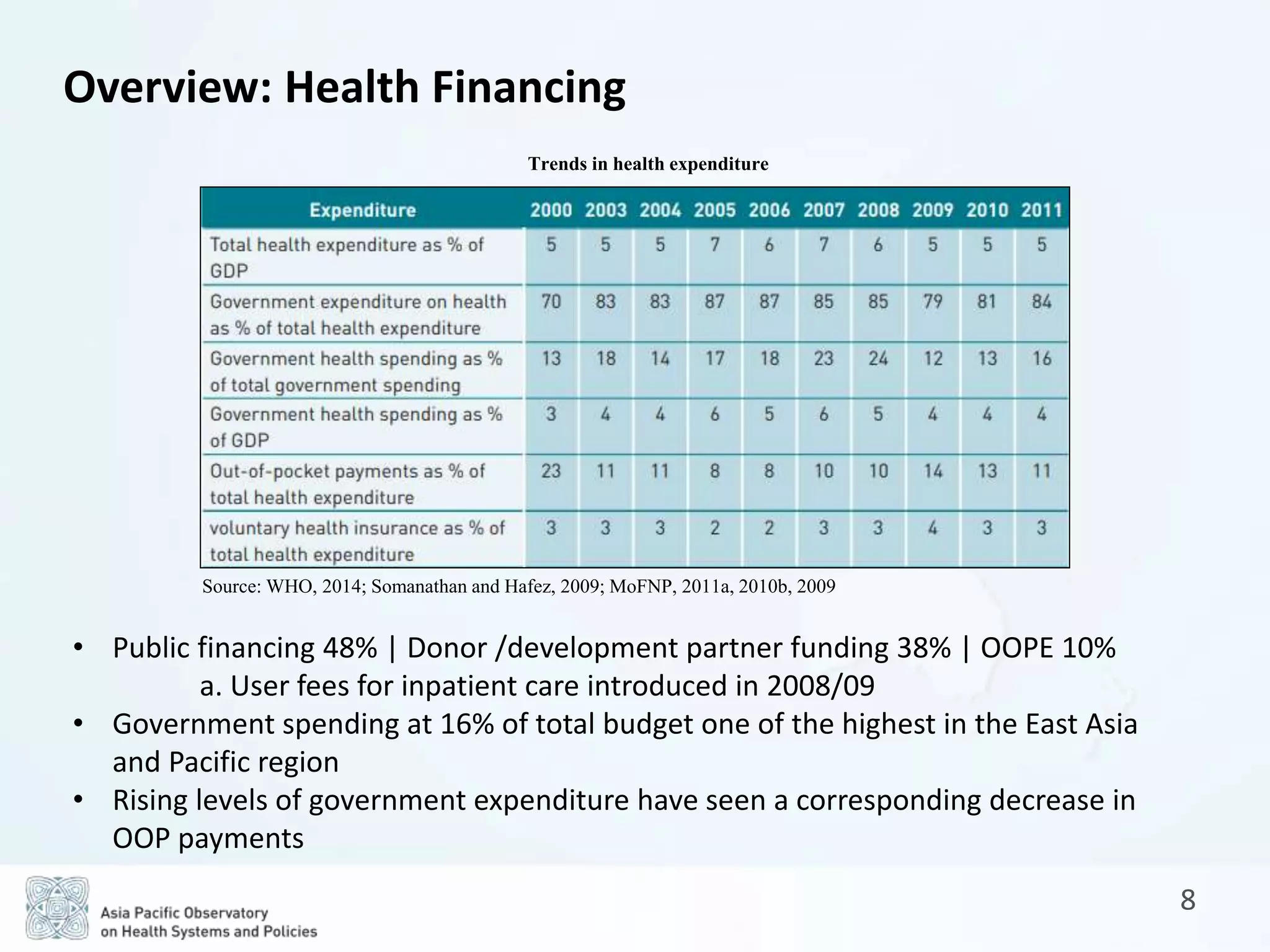
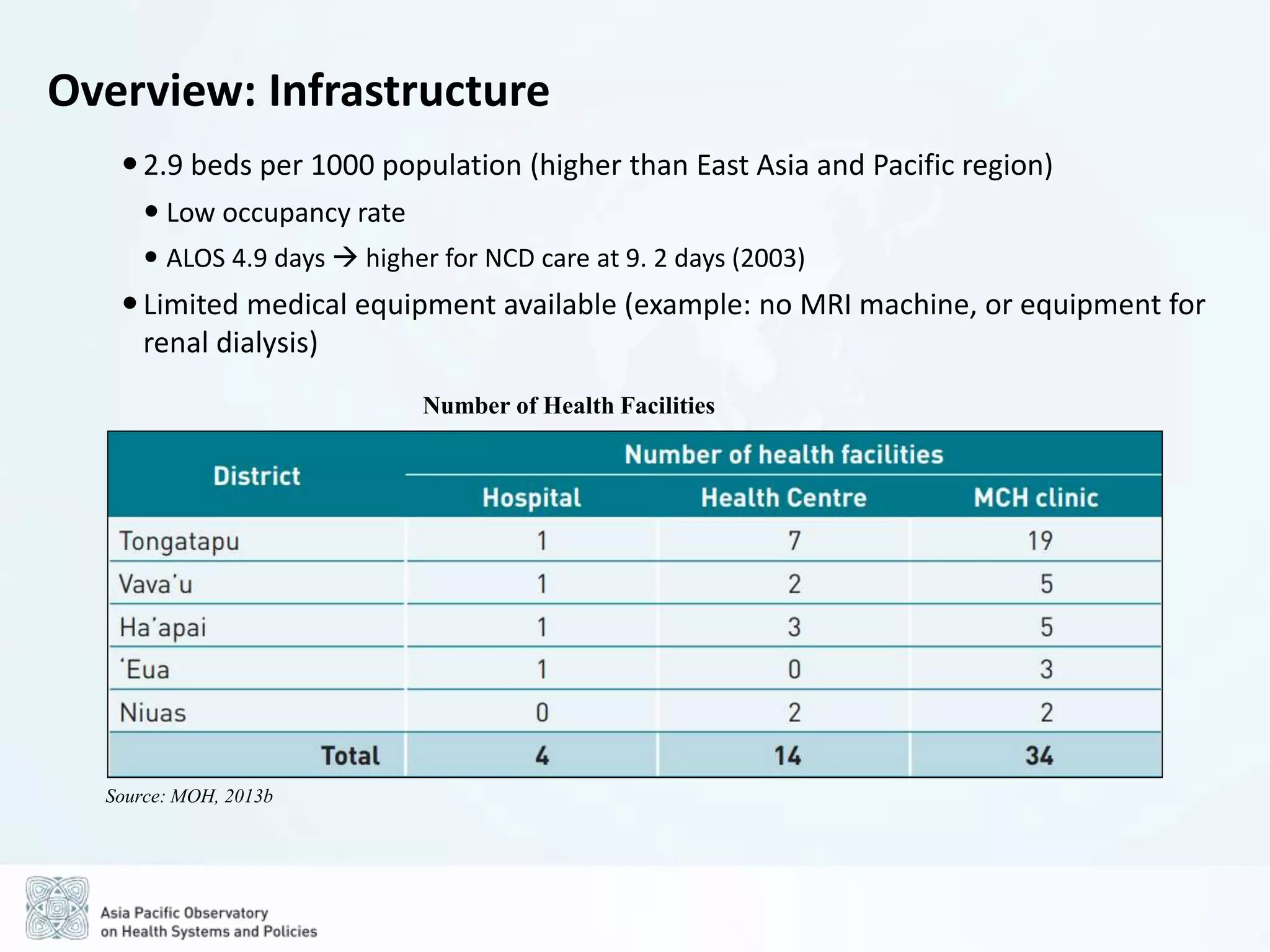
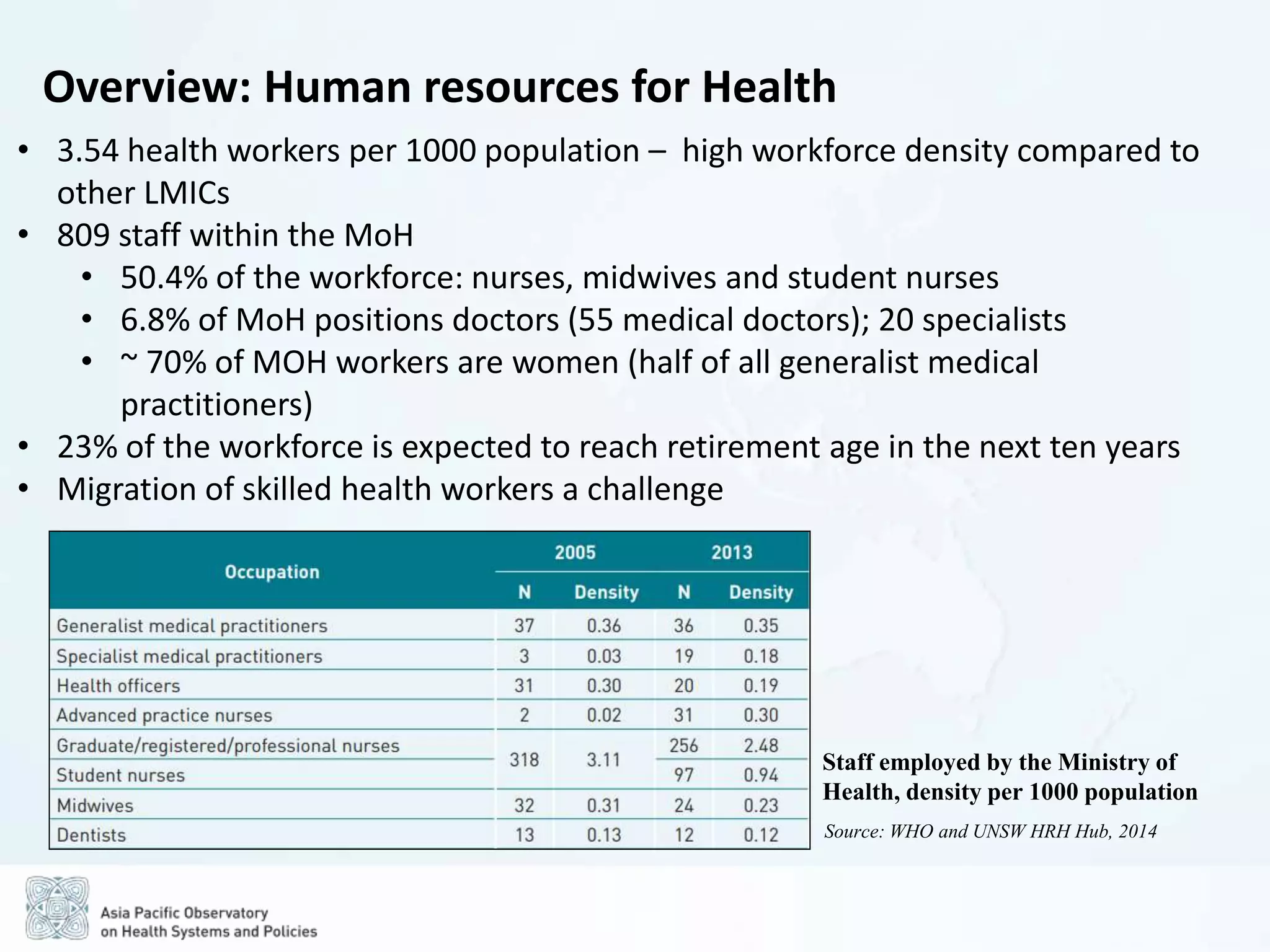
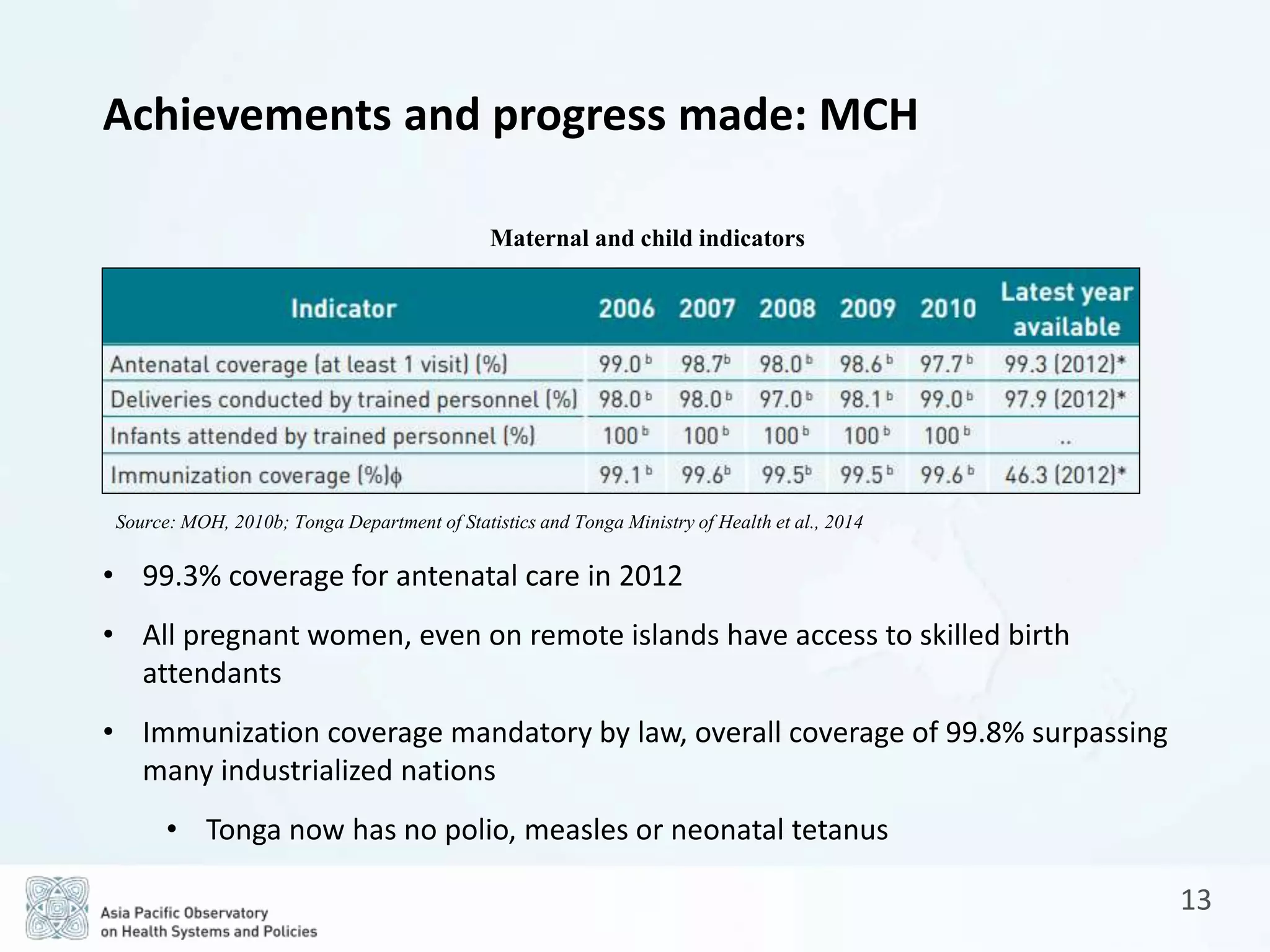
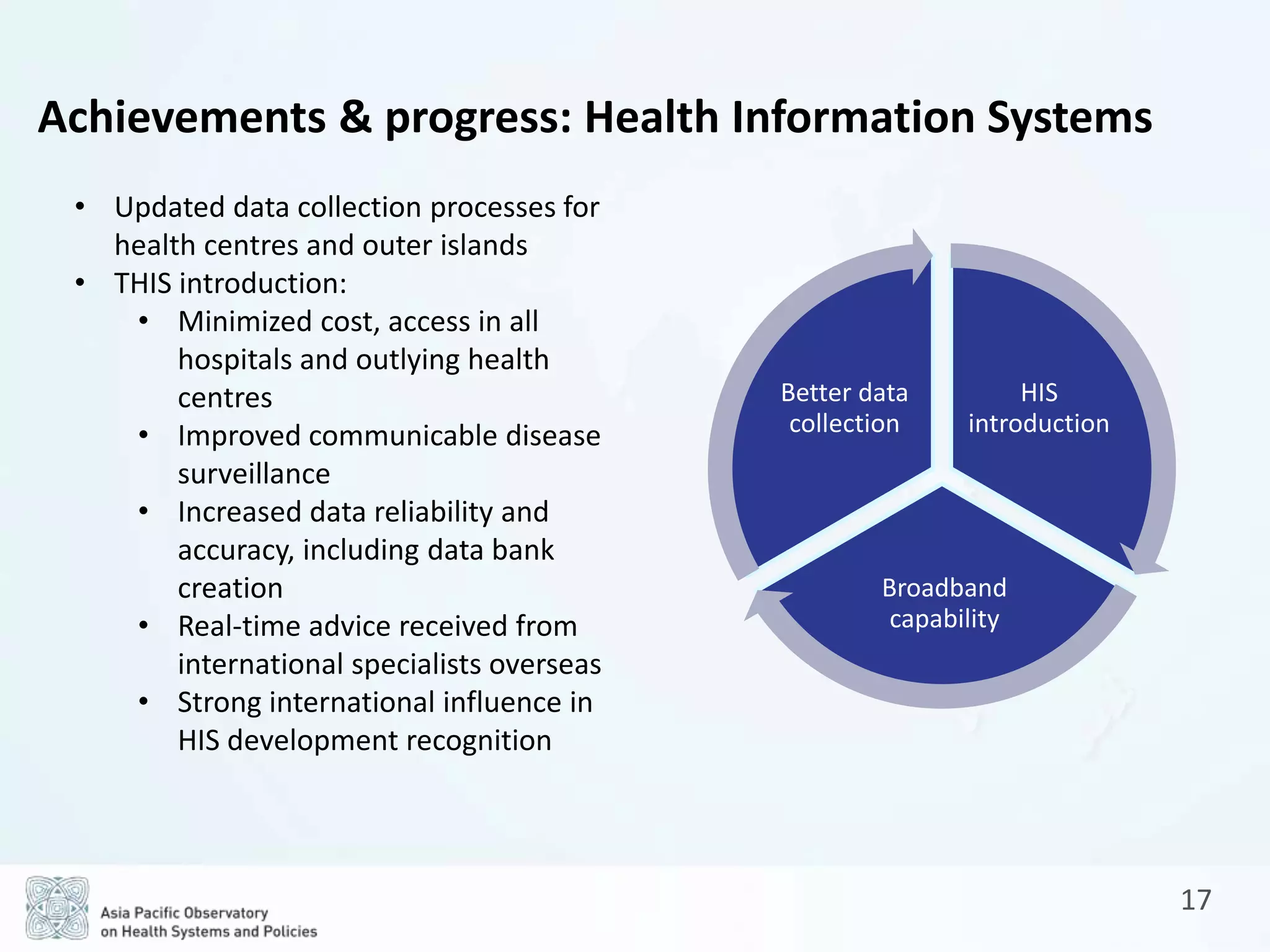
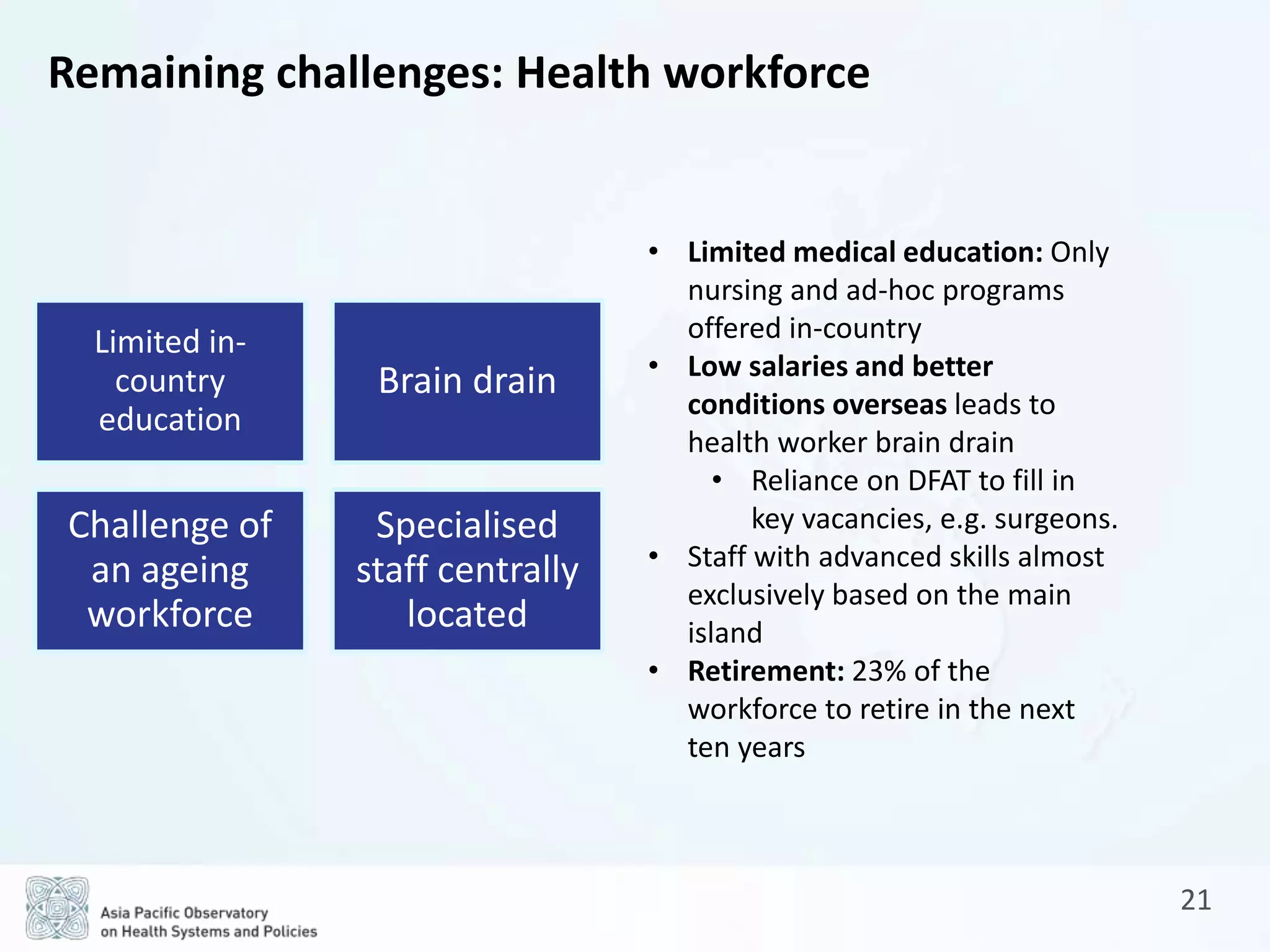
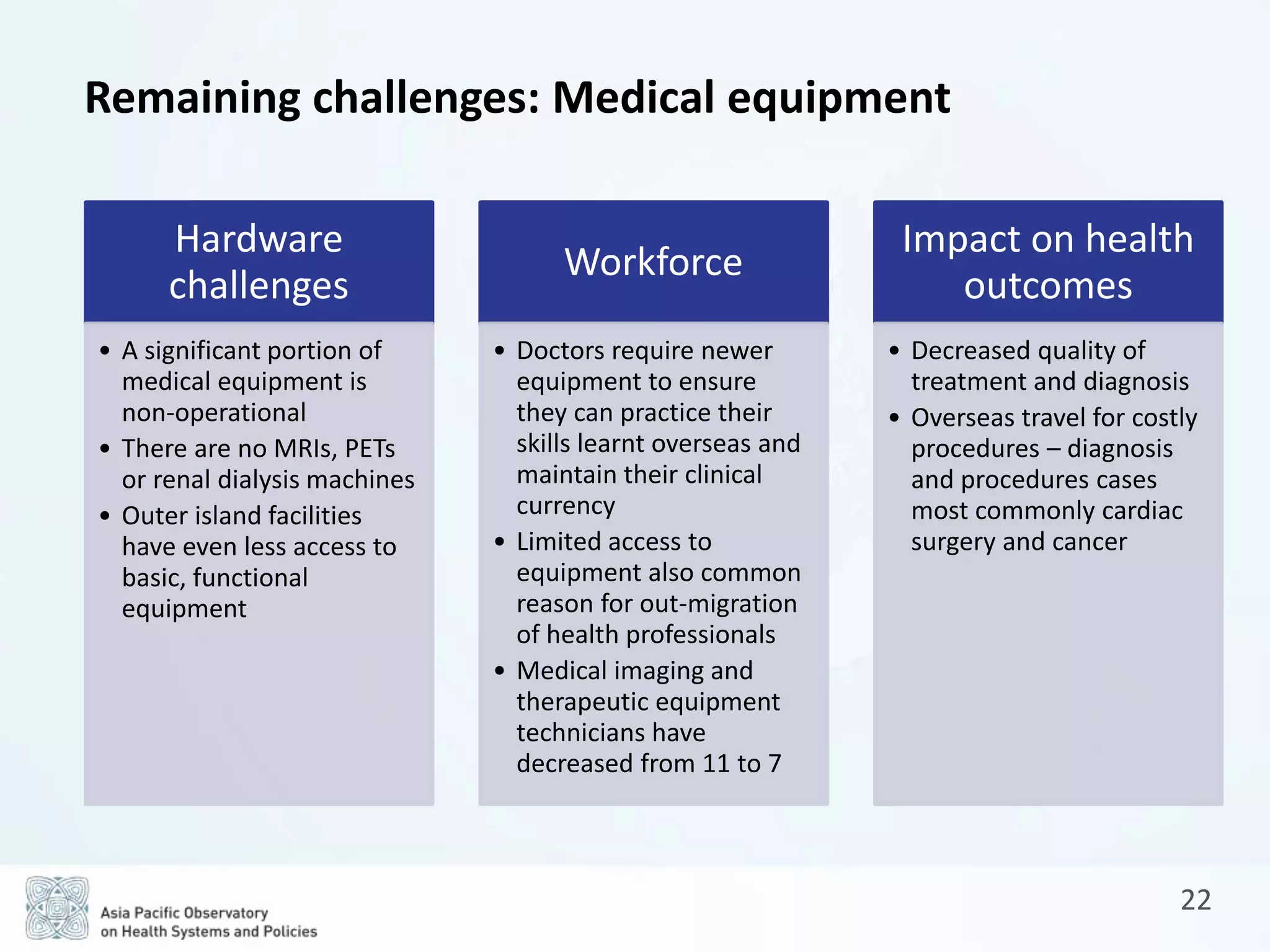
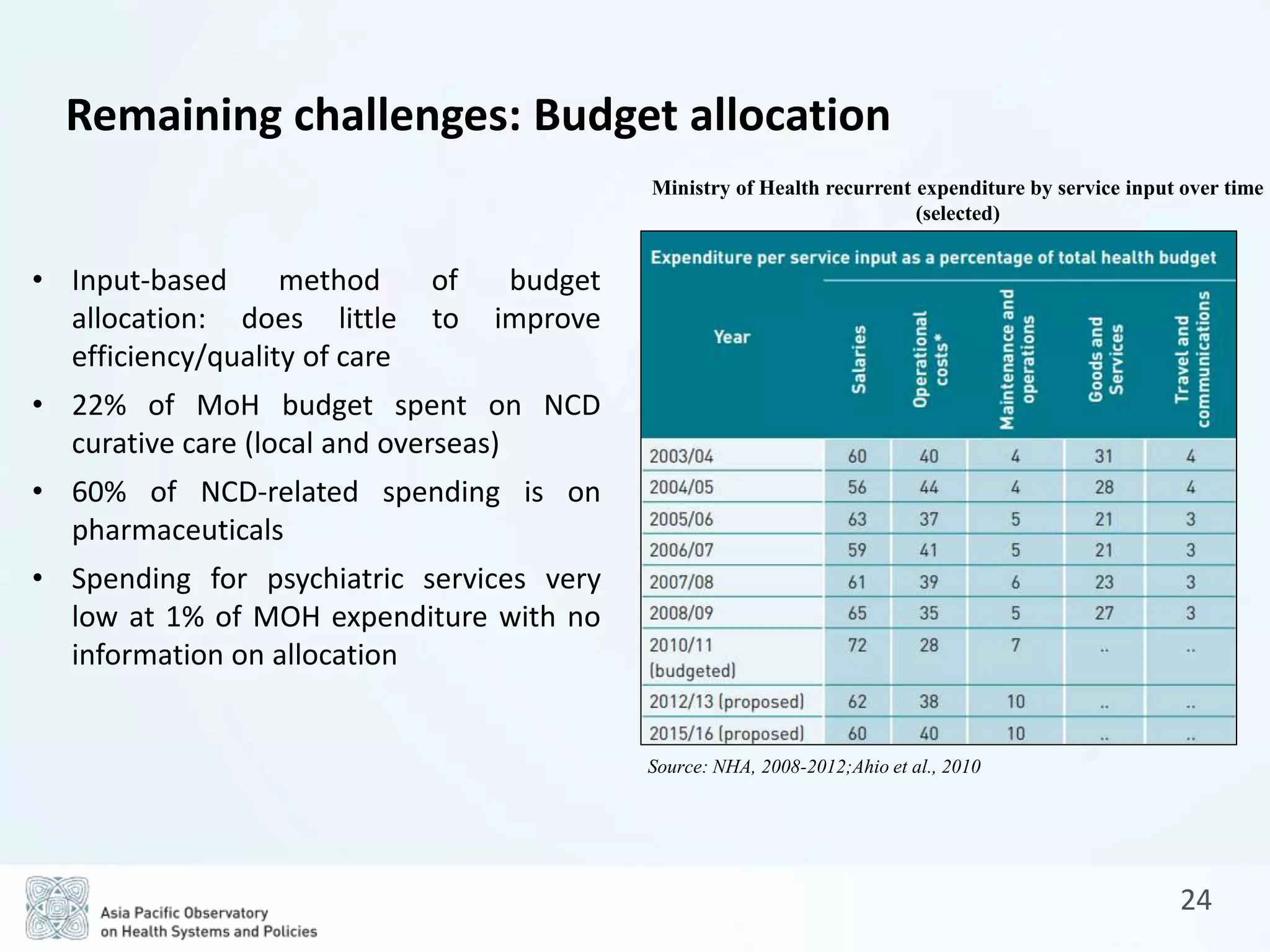
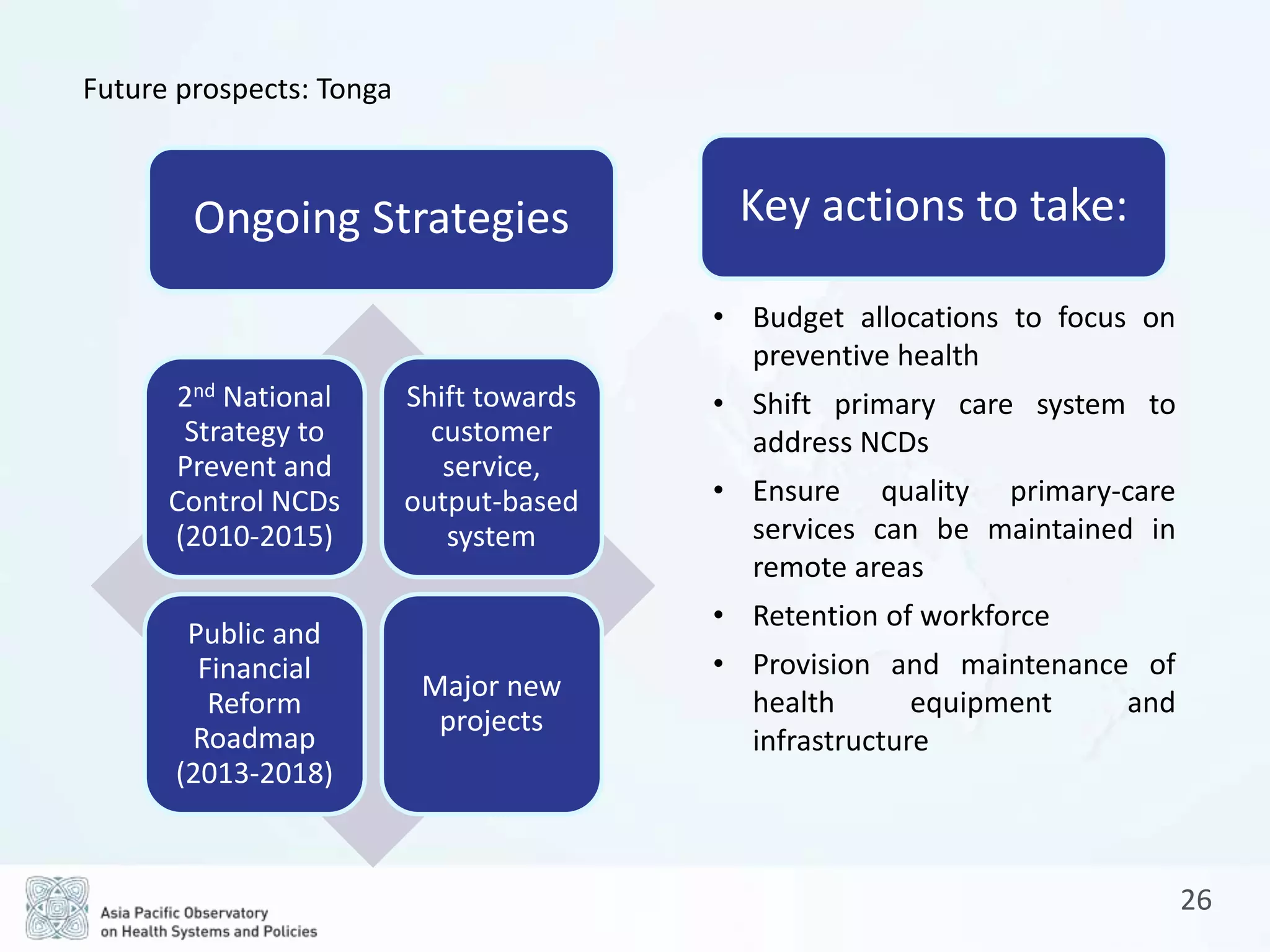
The document is a comprehensive review of the health system in the Kingdom of Tonga, detailing its socio-demographic profile, health service delivery, governance, human resources, and health financing. It highlights achievements in maternal and child health, control of infectious diseases, and focuses on the challenges posed by non-communicable diseases (NCDs) and infrastructure limitations. Future prospects emphasize the need for reforms in budget allocation, preventive health, and workforce retention to improve health outcomes.