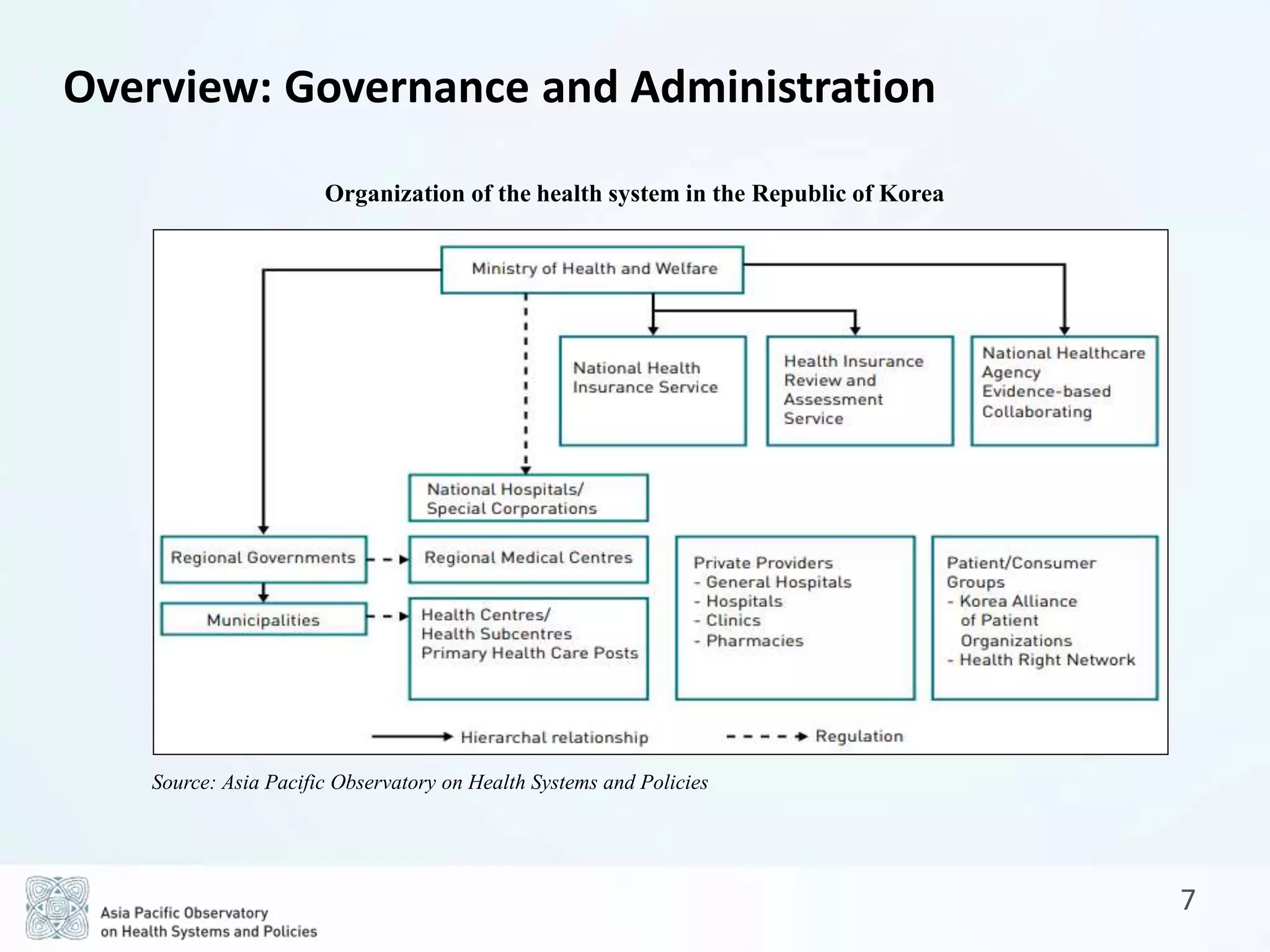
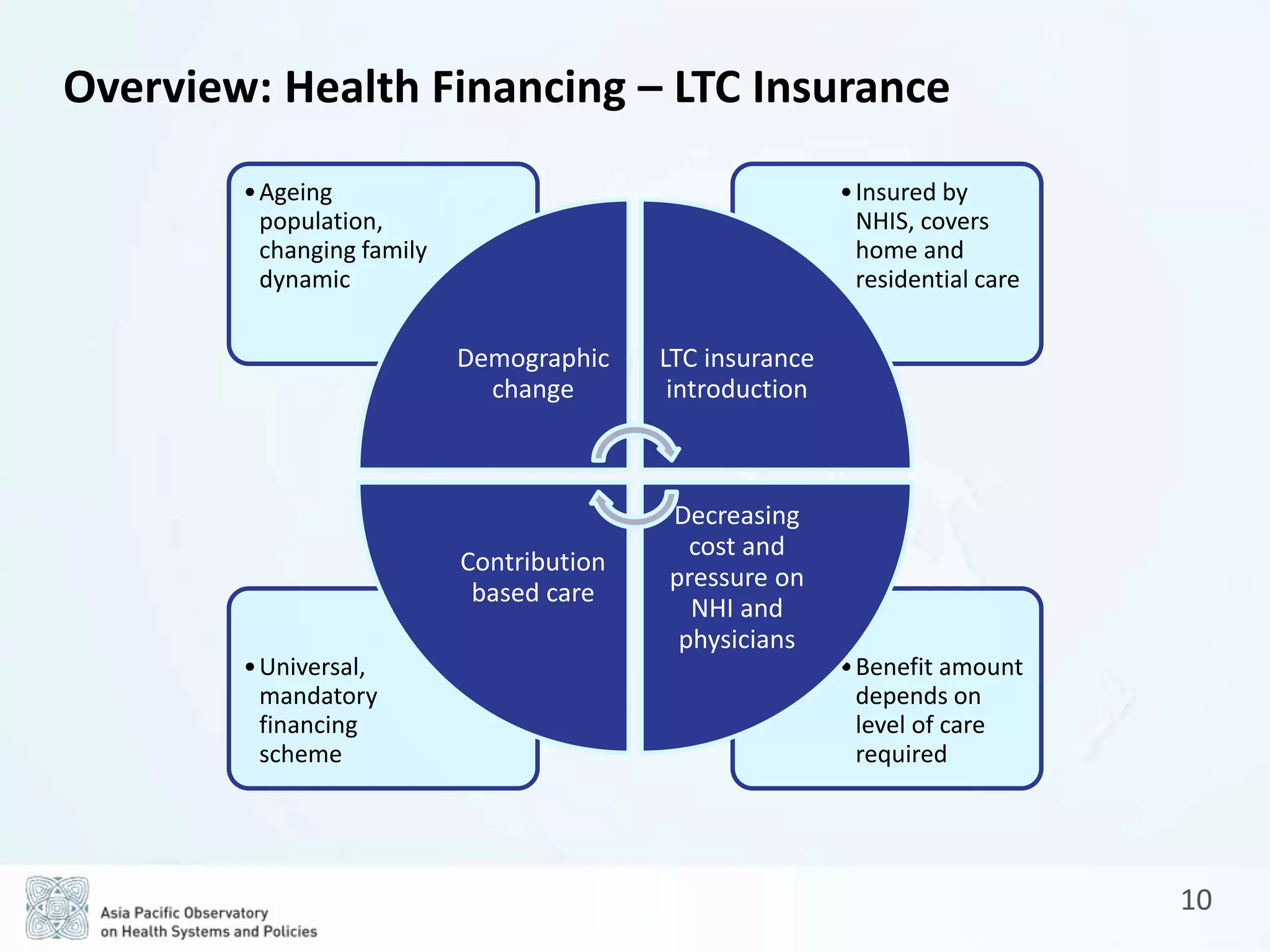
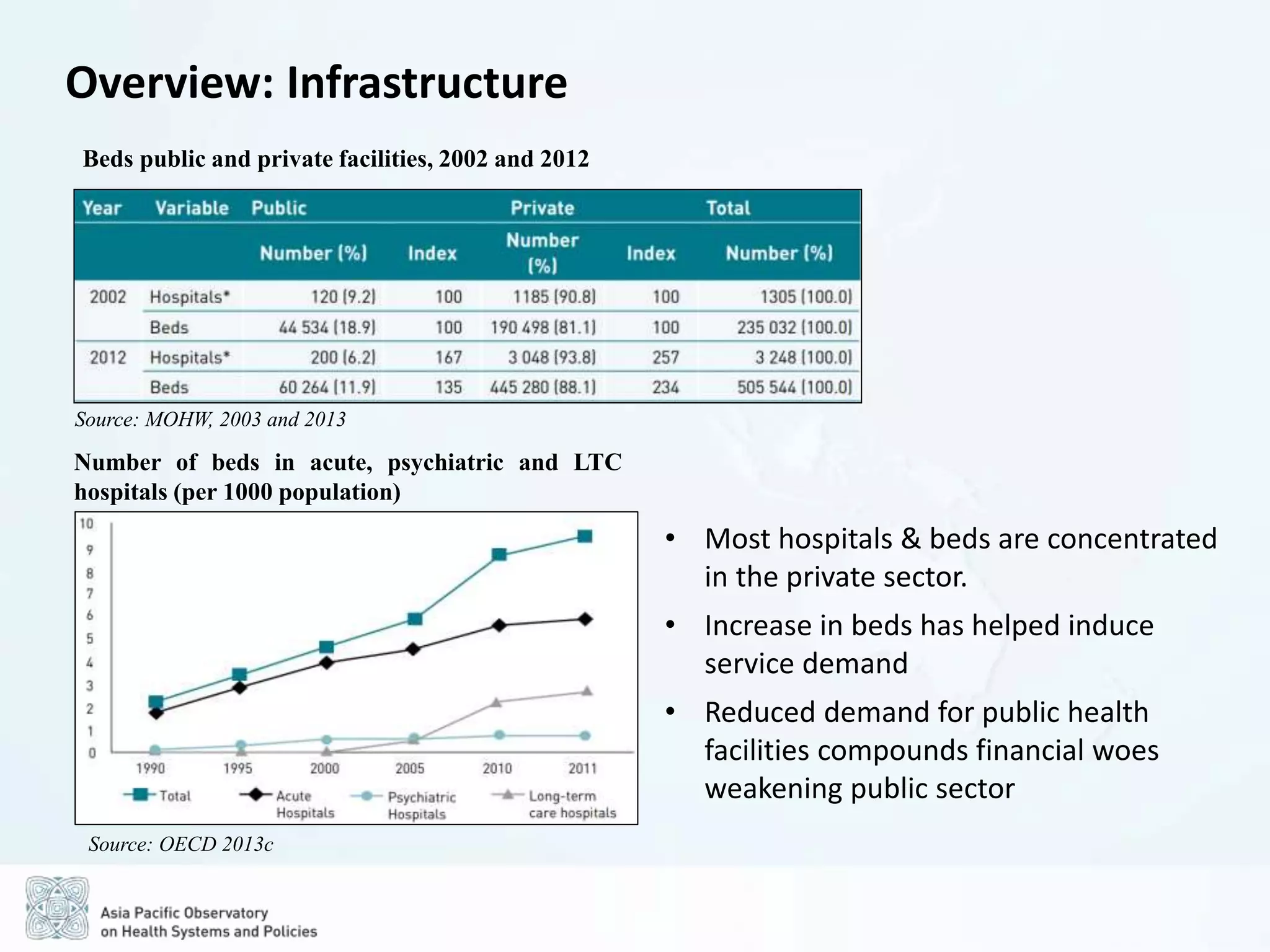
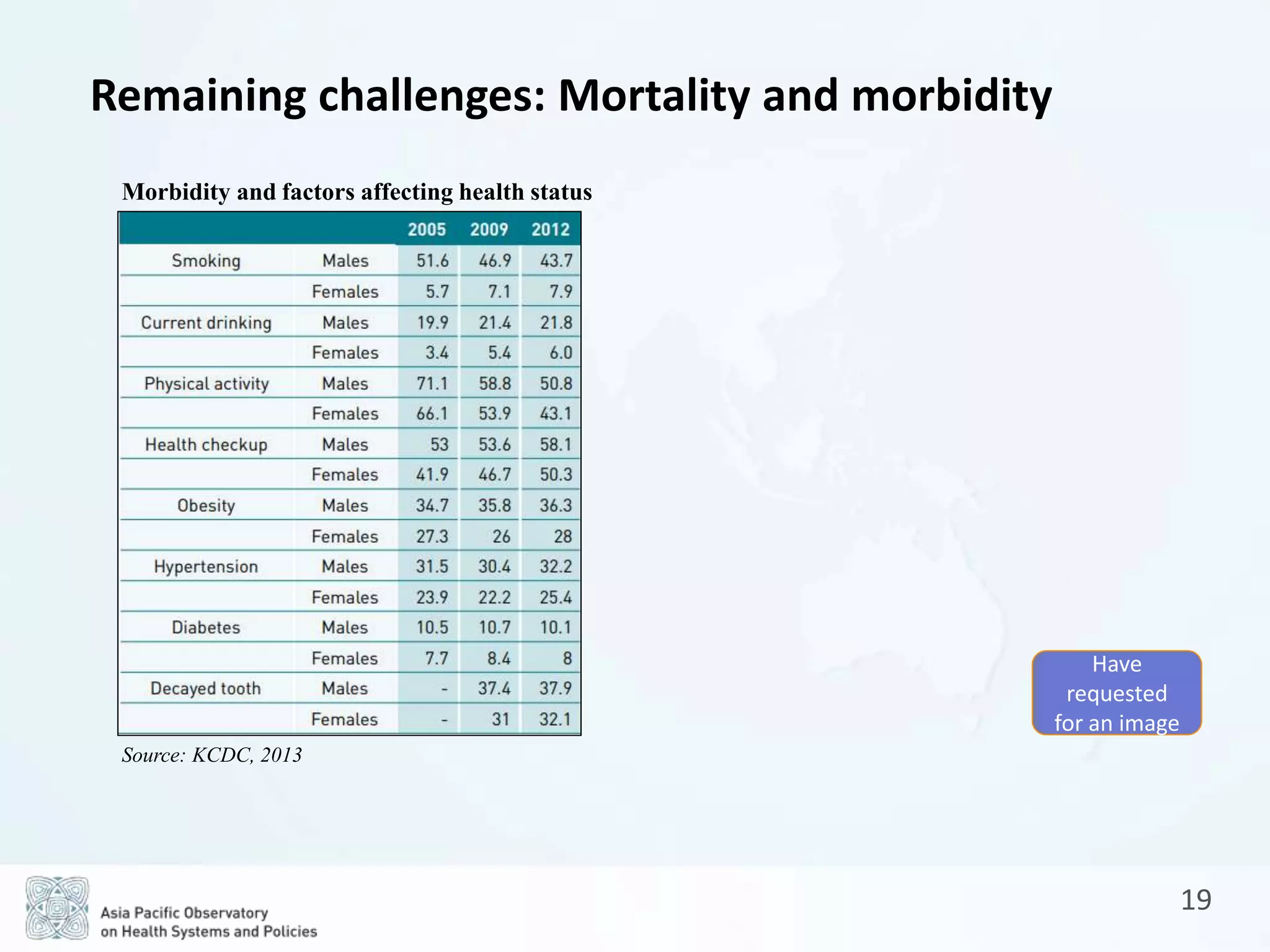
The document is a comprehensive review of the Republic of Korea's health system, covering socio-demographic profiles, health service delivery, governance, financing, and outcomes. Key findings highlight the reliance on a private sector-driven system, the evolution of universal health coverage, and the challenges related to non-communicable diseases and high out-of-pocket payments. It also outlines future prospects for reform aimed at reducing inequities and improving coordination between health insurance and long-term care.