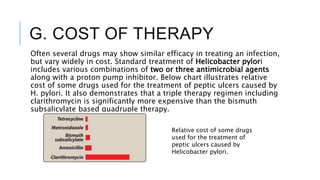
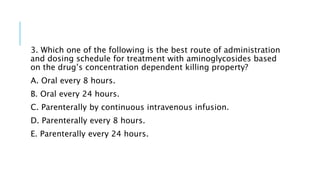
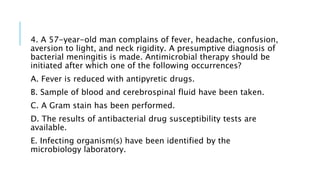
This document discusses antimicrobial drugs and their use. It covers topics like how antimicrobials work by targeting differences between microbes and human cells, how to select the appropriate antimicrobial by identifying the infecting organism and determining drug susceptibility, and factors that influence antimicrobial use like the infection site, patient characteristics, safety, and cost of the drug. Rational dosing based on pharmacodynamics and pharmacokinetics is also discussed.
![2. Renal dysfunction:
Poor kidney function (10 percent or less of normal) causes
accumulation of antibiotics that would be otherwise be eliminated.
Dosage adjustment prevents drug accumulation and therefore
adverse effects.
Serum creatinine levels are frequently used as an index of renal
function for adjustment of drug regimens.
However, direct monitoring of serum levels of some antibiotics (for
example, aminoglycosides) is preferred to identify maximum and
minimum values. Rising minimum values alert the physician to
potential toxicity.
[Note: The number of functioning nephrons decreases with age. Thus,
elderly patients are particularly vulnerable to accumulation of drugs
eliminated by the kidneys. Antibiotics that undergo extensive
metabolism or are excreted via the biliary route may be favored in
such patients.]](https://image.slidesharecdn.com/anti-microbialsnew-230405104306-a2803b27/85/Anti-microbials-therapy-and-complications-pptx-14-320.jpg)
![F. SAFETY OF THE AGENT
Many of the antibiotics, such as the penicillins, are among the least
toxic of all drugs because they interfere with a site unique to the
growth of microorganisms.
Other antimicrobial agents (for example, chloramphenicol) are less
microorganism specific and are reserved for life-threatening
infections because of the drug’s potential for serious toxicity to the
patient. )
[Note: As discussed above, safety is related not only to the inherent
nature of the drug, but also to patient factors that can predispose
one to toxicity.]](https://image.slidesharecdn.com/anti-microbialsnew-230405104306-a2803b27/85/Anti-microbials-therapy-and-complications-pptx-19-320.jpg)