This document discusses principles of antibiotic therapy and treatment of infections. It covers:
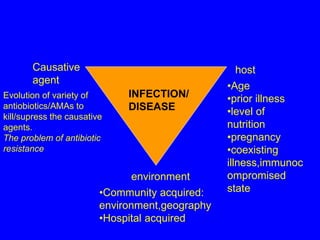
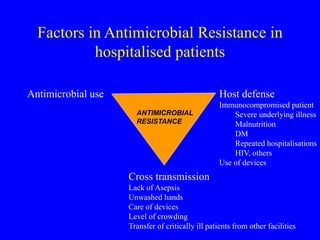
- Factors that influence infection like the host, environment, and causative agent
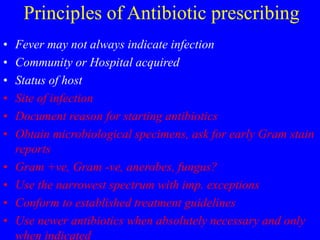
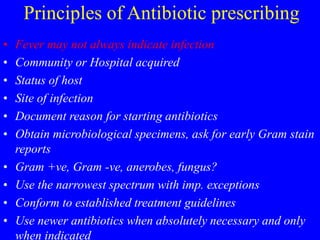
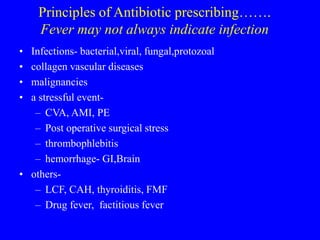
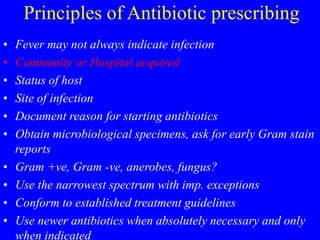
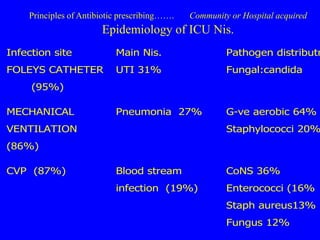
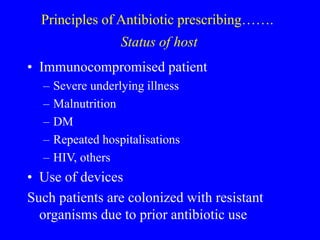
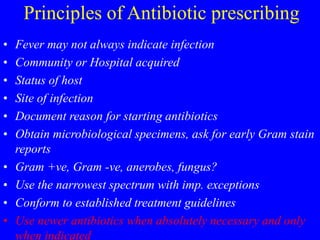
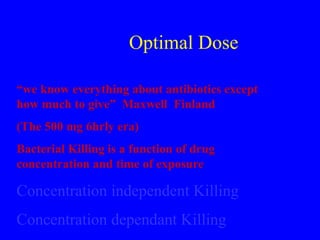
- Principles of antibiotic prescribing including obtaining cultures, using the narrowest effective spectrum, and conforming to treatment guidelines
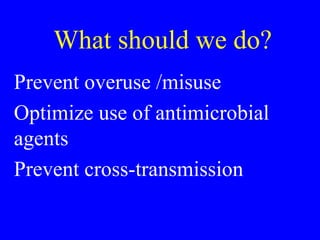
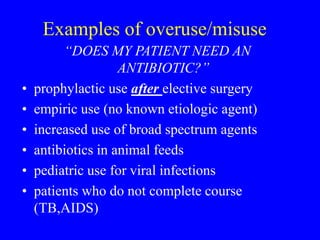
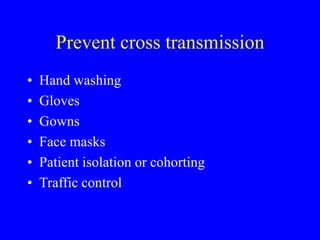
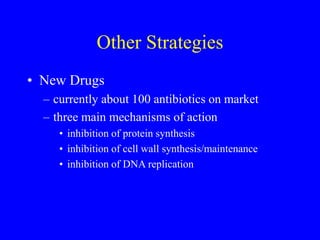
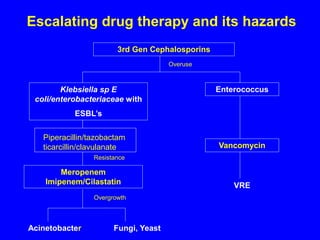
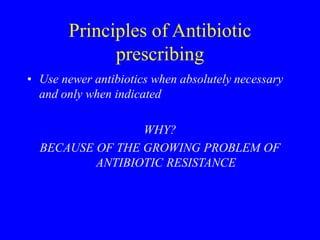
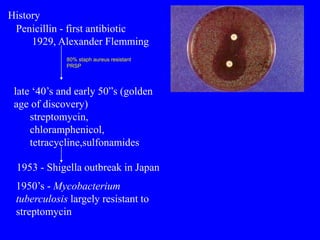
- The growing problem of antibiotic resistance due to overuse and misuse of antibiotics
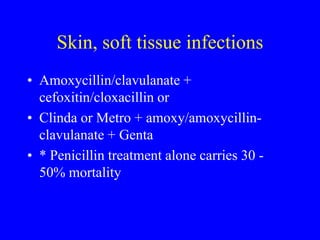
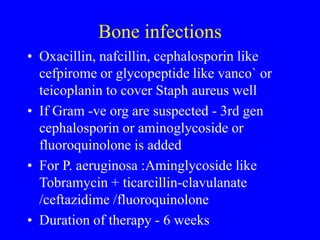
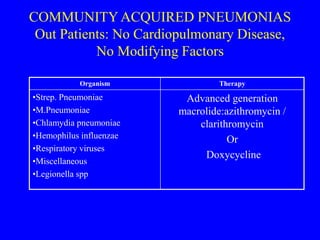
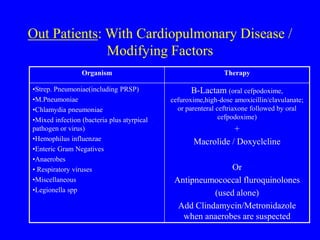
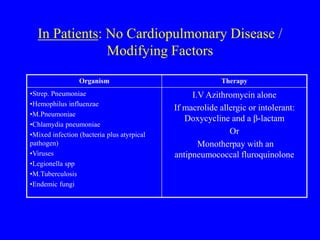
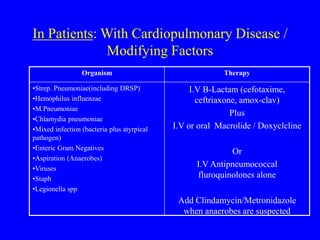
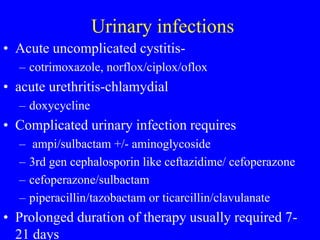
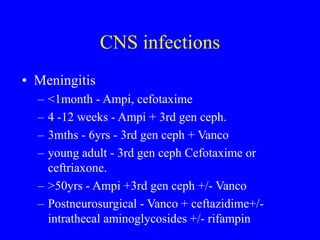
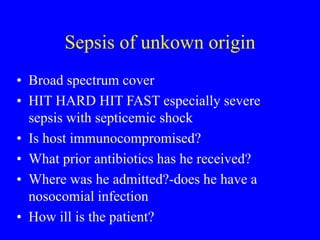
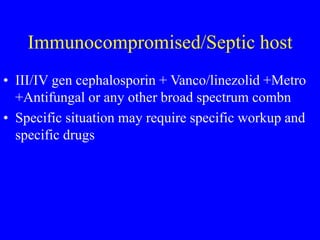
- Examples of optimal treatment for different types of infections like community-acquired pneumonia, bone infections, and skin/soft tissue infections


![Evolution of Antimicrobial Resistance
in Gram-Positive Cocci
S. aureus
Penicillin
[1940s] Penicillin-resistant
S. aureus
Methicillin
[1960s] Methicillin-resistant
S. aureus (MRSA)
Vancomycin-resistant
enterococcus (VRE)
Vancomycin
[1997]
Vancomycin
(glycopeptide)
intermediate-resistant
S. aureus
Vancomycin-
resistant
S. aureus
Ciprofloxacin
1987
[2002]
Adapted from: CDC. Prevent Antimicrobial Resistance: A Campaign for Clinicians. April 2002.](https://image.slidesharecdn.com/antibioticprinciples-230313133344-03f1123f/85/antibiotic-principles-ppt-22-320.jpg)