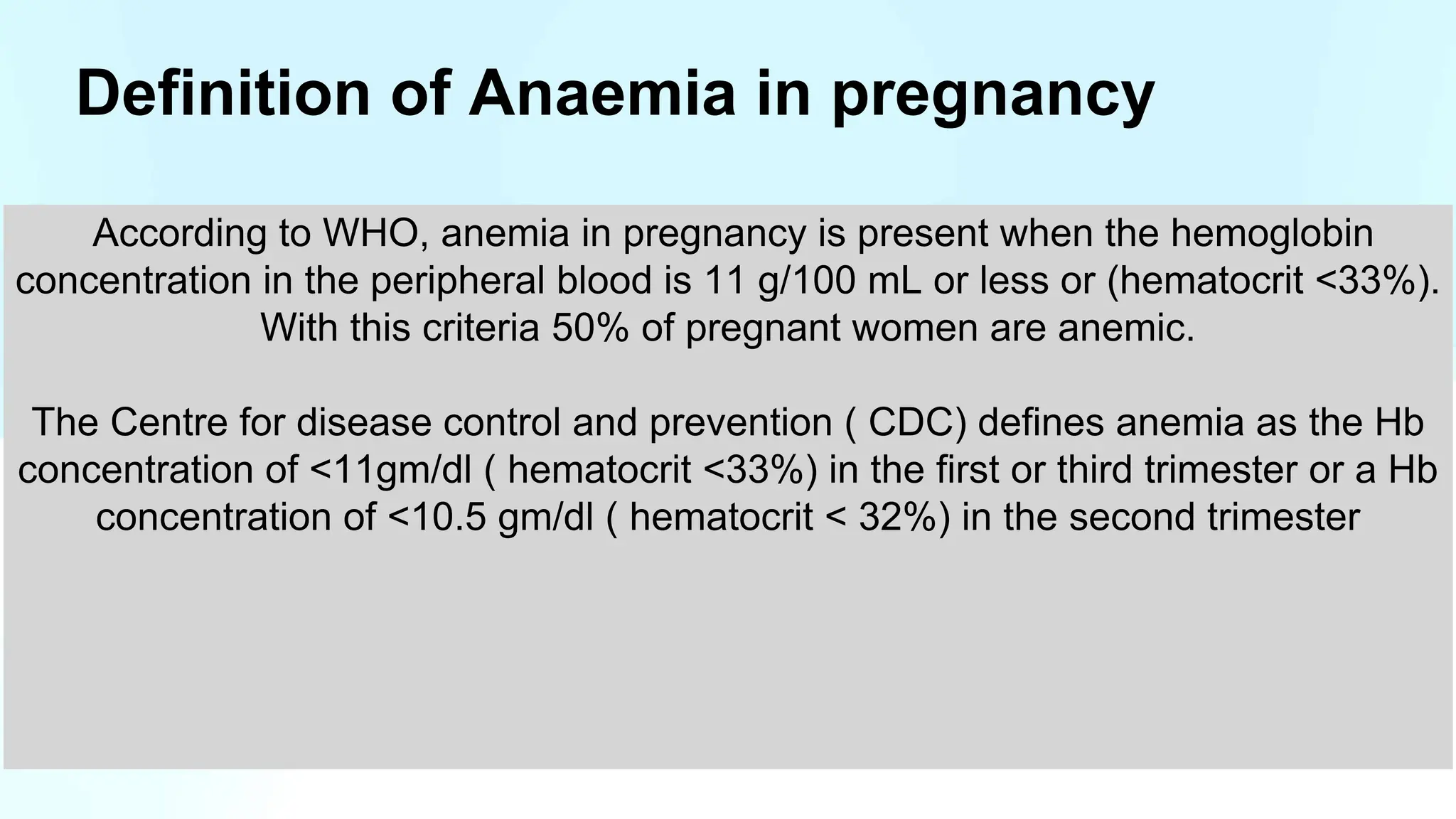
The document discusses anemia in pregnancy, detailing its definitions, classifications, causes, symptoms, and treatment options. It highlights the physiological and pathological types of anemia, the importance of iron and nutrient intake, and management strategies, including prophylactic measures and dietary recommendations. Additionally, it emphasizes the impact of various anemias, such as megaloblastic anemia and thalassemia, on pregnancy and the need for careful monitoring and treatment.









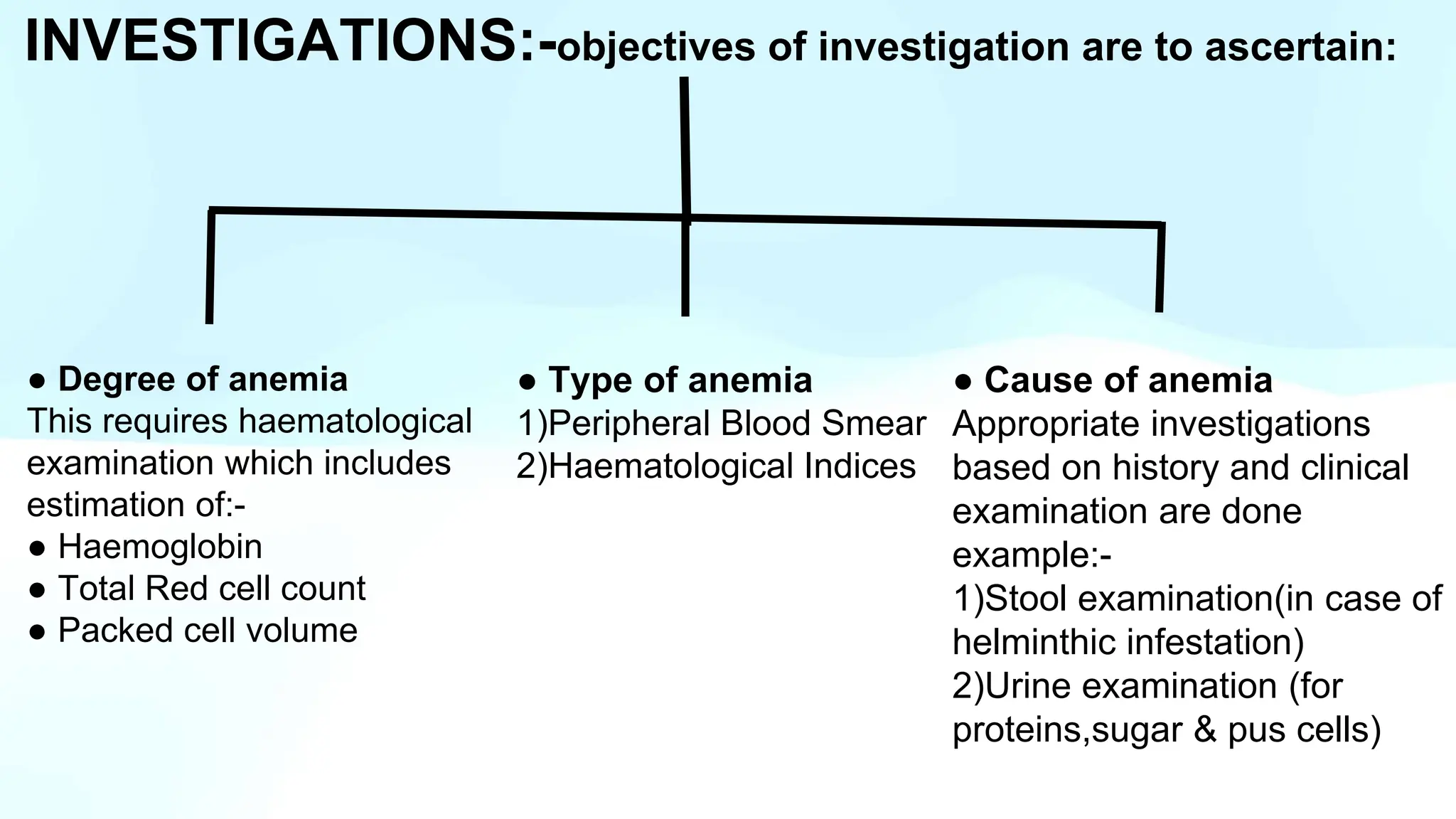











![ESTIMATION OF TOTAL IRON REQUIREMENT USING GANZONI FORMULA:
Total dose of iron required( mg) = body weight in kg( pre pregnancy weight) x [target
Hb - actual Hb gm/L] x 2.4 + 500 mg ( additional to replenish the stores)
Iron sucrose
Max single dose 200 mg
Max iron sucrose/ week 600 mg ( 3 times/ week)
1 vial contains 5 ml/100 mg iron sucrose (1ml = 20 mg of iron sucrose)
Rate of iv infusion= 2 vials (200 mg diluted with 100 ml of normal saline) over 30 min](https://image.slidesharecdn.com/presentation-1-240719052839-9bfda462/75/Anemia-in-pregnancy-definition-causes-pathogenesis-management-23-2048.jpg)

















