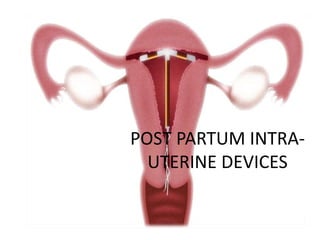
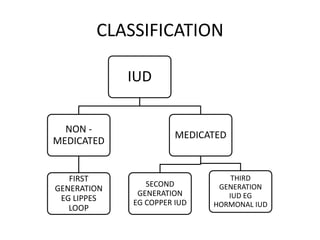
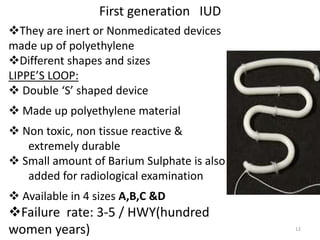
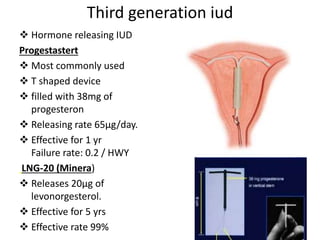
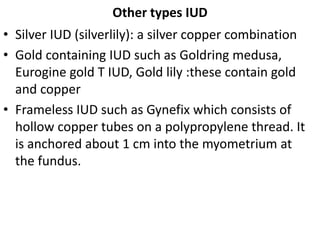
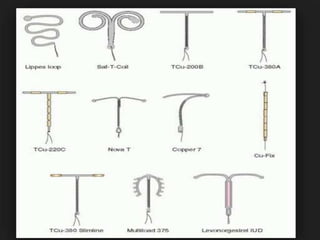
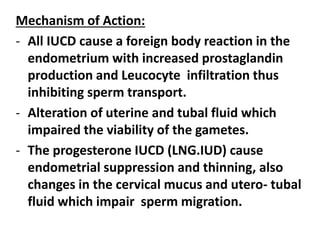
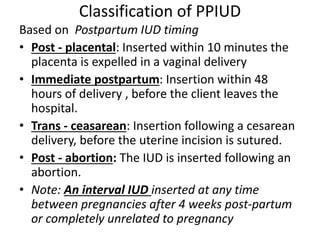
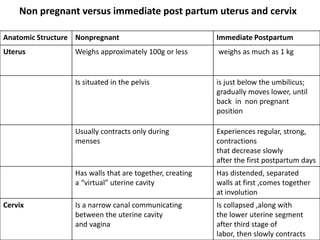
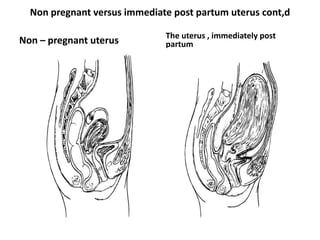
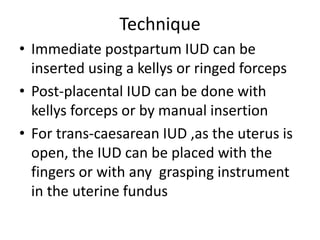
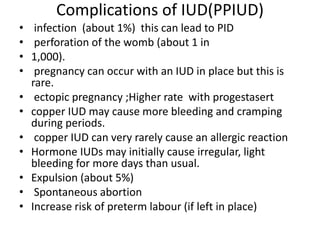
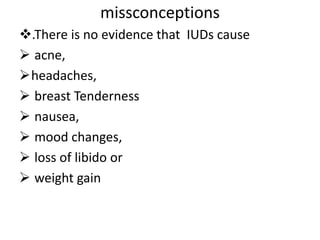
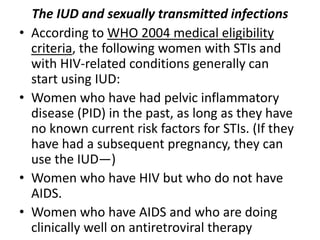
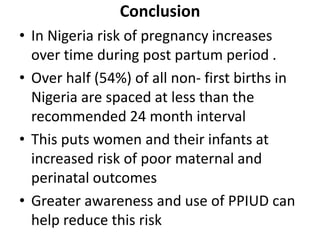
Post-partum intrauterine devices (IUDs) provide safe, effective long-term contraception without interfering with breastfeeding. The document discusses the types and mechanisms of IUDs and the benefits of post-partum insertion. Post-partum IUD insertion can occur immediately after vaginal or cesarean delivery while the uterus is still enlarged, making it easier than non-pregnant insertion. Providers must obtain informed consent and provide counseling and follow-up to clients choosing this method.