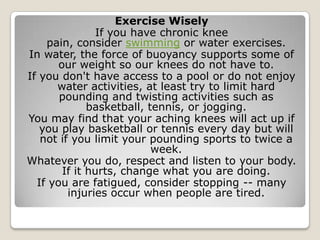
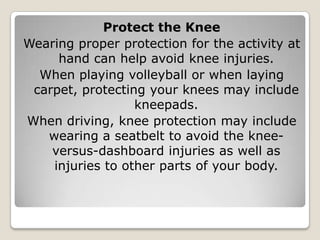
The document provides an overview of the anatomy of the knee, including the bones, ligaments, tendons, cartilage, and bursae. It then discusses common causes of acute and chronic knee pain such as injuries to the ACL, meniscus, and tendons. It outlines treatments for various conditions including PRICE therapy, surgery, and rehabilitation. The document emphasizes the importance of maintaining a healthy weight and lifestyle to prevent knee problems through exercises, stretching, and limiting high-impact activities.